
Collaborative, patient-centred care delivered by interprofessional clinical teams is known to improve healthcare efficiency, as well as patient and staff satisfaction [1]. Therefore, inclusion of interprofessional education as an accredited element within prequalifying healthcare programmes is growing [2]. The use of simulation-based learning may provide an effective method of delivering high quality, safe and effective interprofessional education in challenging but transferable settings like caring for patients presenting with mental health difficulties.
A half-day simulation course consisting of three scenarios was designed. Actors trained in the portrayal of mental health difficulties by service users were workshopped into the scenarios, with representation from each professional group to enhance authenticity. Each scenario was followed by a facilitated debrief that allowed for whole group learning, using a debrief model [3]. Effective interprofessional collaboration and professional representation was modelled by an interprofessional faculty. Facilitators were encouraged to reflect on their own biases around other professions, recognizing the impact these may have on their debriefing choices. During debriefing, participants were encouraged to consider the impact that collaborative practice has on patient-centred care. Facilitators were encouraged to draw out unconscious biases and highlight issues that can inhibit the successful delivery of collaborative, patient-centred care. Staff development was supported through mentorship and faculty debriefing.
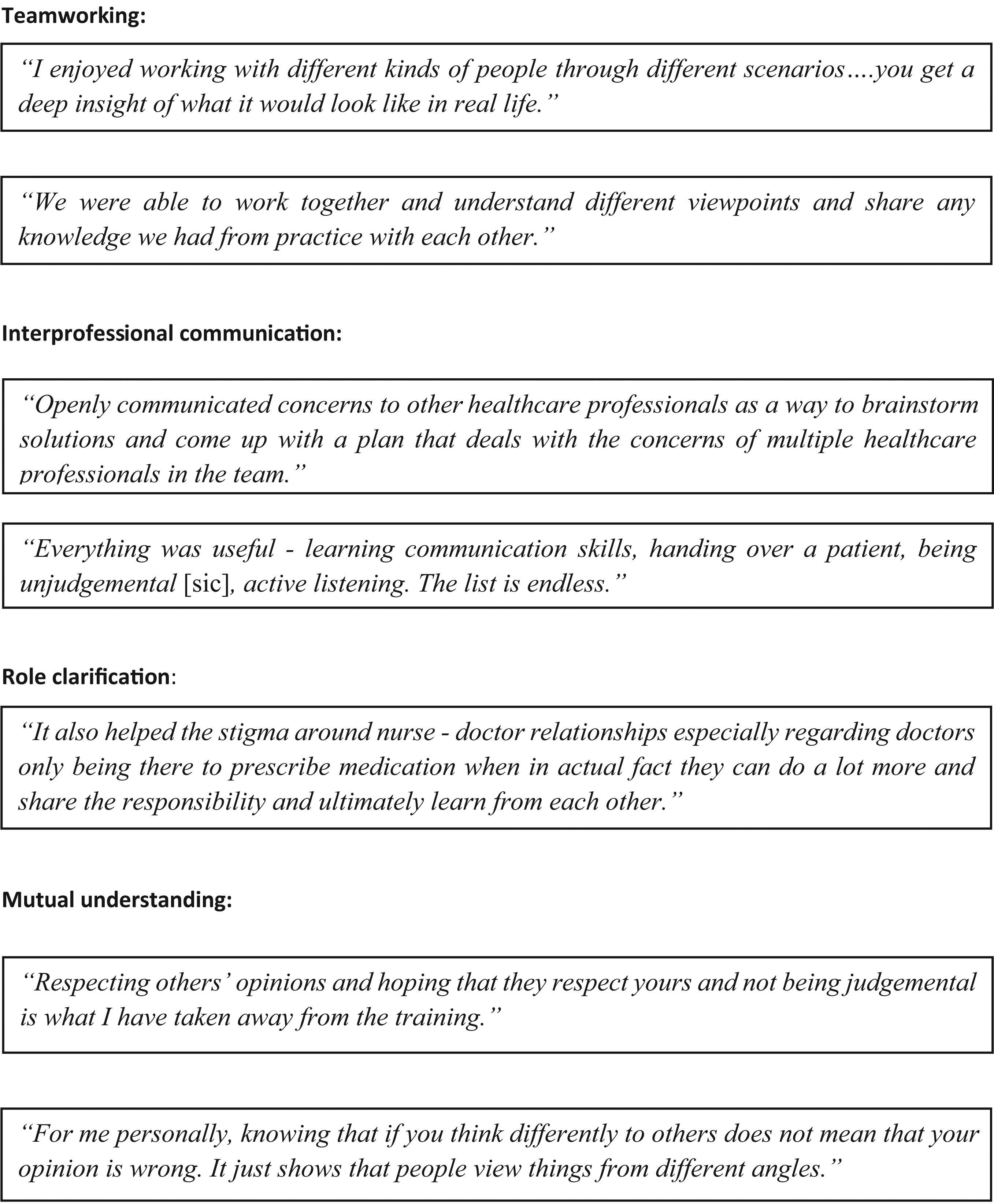
The pilot programme ran four times for 72 nursing and medical students. 50 of the 72 (69%) participants provided anonymous feedback via a mixed methods questionnaire. Of these, 54% were medical students and 46% were nursing students. On a Likert scale (1 = poor, 10 = excellent), all participants rated the experience 7/10 or above, with 74% rating it 9 or 10/10. Likert scale questions regarding applicability, course design elements and perceived learning were also highly rated. Thematic analysis was used to analyse the free text questions by two discrete researchers. The results were broadly categorized into learner experience and learning outcomes. Participant perspectives of the benefits of the simulation training on aspects of interprofessional collaboration can be seen in Figure 1-A64.

This pilot demonstrates that interprofessional education can be successfully delivered in this way, and has been adopted into the medical and nursing student curricula. The next run includes 300 students from medical, nursing and allied health programmes across two institutions, and will be re-evaluated. A qualitative research study to explore the learning that higher educational institutions can gain by delivering interprofessional learning using simulation is also underway.
Authors confirm that all relevant ethical standards for research conduct and dissemination have been met. The submitting author confirms that relevant ethical approval was granted, if applicable.
1. Guraya SY, Barr H. The effectiveness of interprofessional education in healthcare: A systematic review and meta-analysis. Kaohsiung J Med Sci [Internet]. 2018;34(3):160–5. Available from: https://doi.org/10.1016/j.kjms.2017.12.009
2. CAIPE. Centre for the Advancement of Interprofessional Education Strategy 2022 – 2027. 2022. Available from: https://www.caipe.org/strategy#1
3. Jaye P, Thomas L, Reedy G. ‘The Diamond’: a structure for simulation debrief. Clin Teach. 2015 Jun 25;12(3):171–5. Available from: https://onlinelibrary.wiley.com/doi/10.1111/tct.12300