
Simulation is an effective educational strategy to train those caring for older adults (persons over 60 years old). Working with simulated participants (SPs), well people trained to portray others, is an appropriate modality when learning objectives relate to behavioural skills. The COVID-19 pandemic has disrupted every aspect of society. At our simulation programme, we implemented a weekly, virtual, 1-hour meeting modelled on a framework that incorporates effective practices in simulation and working with older adults. In this paper, we explored older volunteer SPs’ perceptions of the shift from in-person to virtual meetings and its impact on their well-being and SP skill development.
This was a qualitative exploratory study of older adult SPs’ experiences within the virtual SP meetings. Thirteen volunteer older SPs consented to participate in audio recorded focus groups where they were asked to describe their experiences with the virtual SP meetings. A collaborative, inductive coding approach was adopted, followed by thematic analysis, aligned with the methods described by Braun and Clarke. Ethics approval was obtained.
Four primary themes were identified: fostering meaningful and cohesive group connections; gaining personal benefits; enhancing SP skills and competence; and appreciating structure.
A structured, regularly occurring virtual meeting is beneficial to the building and maintenance of SP skills for older adults and their well-being. This approach could be applied to other groups of SPs with the proviso that facilitators are skilled, and a framework is in place featuring the basic tenets of effective simulation.
Simulation is an effective educational strategy to train those caring for older adults (persons over 60 years old) [1–5]. Working with simulated participants (SPs), well people trained to portray others, is an appropriate modality when learning objectives relate to behavioural skills [3, 6]. Evidence-based approaches exist for engaging with older SPs in a safe and effective manner. Research shows that working with older SPs promotes authenticity and engagement for learners [7]. Older SPs have also reported benefits including enhanced well-being, building social networks, satisfaction drawing on personal experiences to improve care, feeling appreciated, having a sense of purpose, learning and having fun [8, 9].
As simulation educators at Baycrest (Toronto, Canada), an academic health science centre affiliated with the University of Toronto that provides care for older adults across a variety of institutional and community-based settings, we work with a vital and highly engaged group of older volunteer SPs. This SP group is called ‘SAGE’, which stands for Simulation Activities for Gerontological Education. The COVID-19 pandemic has disrupted every aspect of society, including simulation programmes [10, 11]. Since our in-person learning was suspended in March of 2020, these SPs have experienced prolonged social isolation through fluctuating degrees of lockdowns and social distancing regulations. They expressed that this isolation and inability to contribute through their work as SPs was having a negative impact on their well-being.
After the first lockdown was imposed (April 2020), we implemented weekly, virtual, 1-hour meetings modelled on a framework we created [12] that incorporates effective simulation practices [13, 14] and working with older adults [15–19]. Strategies that promote well-being in older adults such as mindfulness, structured daily activity, discussion, skills development, storytelling and improvisation were included [20–23] . Each week followed the same structure: briefing (via email the day before), social connection, a short mindfulness activity and a storytelling activity, where each SP shared a story around a predetermined theme. Short, facilitated discussions were held between stories. The meetings concluded with a wrap-up. Facilitators debriefed and reflected on their experiences with and learnings from the meeting (see Figure 1, Meeting Framework).

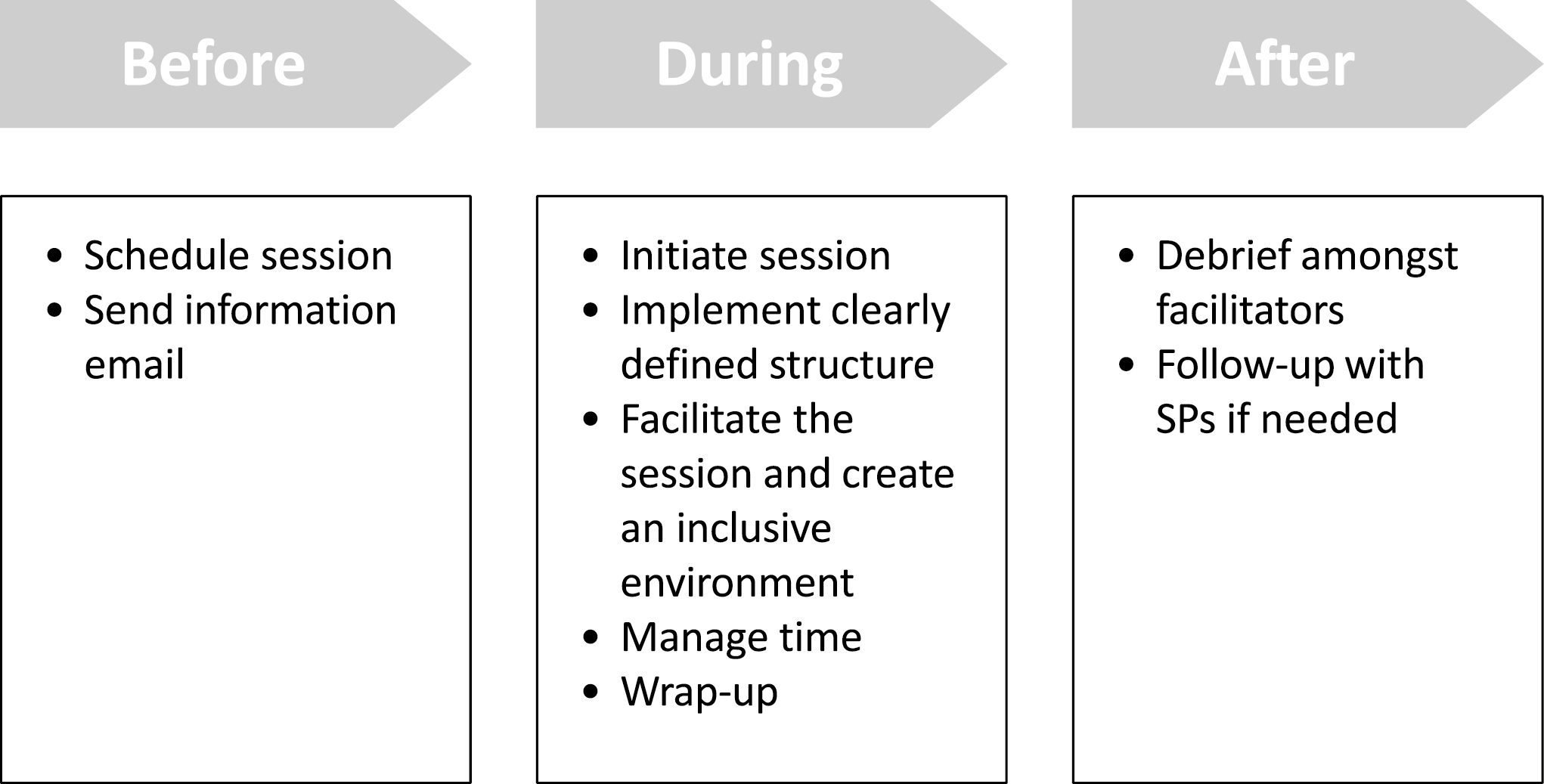
Meeting framework
In this paper, we present the results of a qualitative study evaluating the SPs’ perspectives of the effectiveness of these meetings. We explored older volunteer SPs’ perceptions of the shift from in-person to virtual meetings and its impact on their well-being and SP skill development.
This study adopted a reflexive approach; the group facilitators (LS and CS) have extensive experience in developing and implementing SP programmes. A qualitative researcher not connected to the programme or participants (CG) was involved in data coding and analysis.
This was a qualitative exploratory study of older adult SPs’ experiences with the virtual SP meetings, which spanned a period of 5 months (April–August 2020).
SPs were recruited to the study via convenience sampling. The programme facilitators (LS, CS) approached all older adult SPs taking part in the meetings and invited them to participate. Ethics approval was obtained from the Baycrest Research Ethics Board (REB #16-04). All SPs provided written informed consent to participate.
SPs participated in one of four, 30–45-minute, audio-recorded focus groups where they were asked to describe their experiences with the virtual SP meetings. Focus groups were facilitated by one investigator (CS), who explored the SPs’ experiences using a semi-structured topic guide (Table 1). All audio recordings were transcribed (clean-read verbatim) and uploaded into NVivo v. R1 (QSR International, Doncaster, Australia) for qualitative coding and analysis.

| Interview questions and probes |
|---|
| 1. Do you feel that social distancing during COVID-19 has affected you? |
| a. In what way(s)? |
| b. Please share some examples. |
| 2. With respect to social distancing, how do you feel about our weekly SAGE ZOOM get-togethers? |
| a. Do they add value? |
| b. Do they have an effect on your mental health/ well-being/social connectedness? |
| 3. How do you feel about the following components of the weekly sessions? |
| a. Mindfulness activities? |
| b. Weekly assignments? |
| c. Social conversation? |
| 4. Have you taken anything from this that you can use as an SP? |
| 5. Is there anything else you would like to share? |
A collaborative, tandem, inductive coding approach was adopted [24], where CS and CG generated first-pass codes using an in vivo coding approach [25]. Tandem, collaborative coding promoted reflexivity, as the programme facilitator engaged in active reflections during the coding process based on their experience with the programme, participants and data; these were captured in detailed annotations and memos. CG co-generated codes and verified whether they remained true to the data. Codes were assigned to the data once consensus was reached by both coders. To ensure further rigour and reflexivity, LS verified the coding scheme to ensure that the codes were aligned with the data, and with their own experiences and reflections of the programme.
The data was analysed thematically as described by Braun & Clarke [26]. The themes were further updated following reflexive discussions with the programme facilitators and were aligned with the study objectives and effective practices in SP methodology.
Thirteen participants enrolled in the study. All participants were older adult SP volunteers with an average age of 78.9 years (range: 66–90 years); 77% of participants (n = 10) were female. All SPs had been participating in the in-person programme from 1–5 years.
Four primary themes were identified.
These meetings offered SPs the opportunity to establish or maintain social connections with others in the group, especially since many of their other existing connections had been disrupted by the pandemic. On a very basic level, one SP valued that contact was made.
‘I think meeting here like this was very good for me because I volunteer in another organization … and I feel disjointed from them whereas I feel closer to our [SP] programme now.’
Another SP noted that this participation created greater group cohesion:
‘I am very happy that we did this because it’s keeping our group together.’
When examining this sense of connection more deeply, three key characteristics were identified. First, the SPs valued the companionship that developed between group members because of keeping the SP group together. These participants reported how they appreciated spending time with, engaging in conversations with and learning from others. By participating in the programme, these SPs broadened their social networks:
‘I think we are getting to know each other in a different kind of way than we would normally.’
Second, the SPs appreciated caring about and feeling cared for by others; participating in the group enabled them to support others and receive help from others.
‘… I think everybody cares about everybody else and in this way, we have an ongoing contact, and we can actually see each one of us on an ongoing basis and not be worried that people are falling off the cliff or people are getting ill.’
‘… You can discuss missing your families and we’re all suffering the same way about COVID so we can express ourselves … that’s what you do in a group.’
Finally, some SPs explained how participating in the programme enabled them to develop deep, meaningful and intimate group connections. For these SPs, taking part in the group felt ‘like family’, where they really got to know and felt ‘in tune’ with other SPs. In some cases, the SPs found themselves developing deeper connections with others over the virtual platform when compared with in-person:
‘[The intervention] made a big difference in my life. It’s like it has built a special contact community and it’s more like family. And we get to know each other and we’re sharing things and sharing thoughts and making suggestions that are helpful for each other.’
‘Other people are newer, and I think that this has been … a bit like a crucible it’s kind of intensified a little bit and forced us to talk about things and reveal things and develop even a deeper affection.’
There was also a recognition of the potential powerful impact of this deeper knowing of each other on future in-person SP work:
‘I think it will eventually contribute when we get back to what we used to consider to be normal. It can contribute to the way that we can be SPs because we know each other.’
The SPs derived several personal benefits from attending the meetings, which extended beyond the initial goals of the activity. Some SPs noted how volunteering with the group and ‘paying it forward’ enhanced their mood and well-being, and served as a driver to attend the sessions:
‘I think the sessions are really good way to maintain an equilibrium of thought, social connections for all the participants and in that it’s certainly important and of course with [the] vast majority being seniors, it also adds to our well-being.’
‘[The programme] … it’s like a shot in the arm to continue on in a very exciting way.’
Others gained benefits from specific components of the meetings. They enjoyed the challenge of having ‘to adapt to new ways of doing things’. Some described that the mindfulness component led to a general reduction in stress and nervousness, promoted relaxation and even helped them sleep. Some began incorporating mindfulness activities into their daily lives to achieve a sense of calm, relaxation, and focus.
‘I think that those little mindfulness exercises are really quite helpful as an introductory relaxation thing. … I think what it does… it allows people to just open just a little bit more perhaps and get ready to share, you know they are more relaxed.’
‘I have never done successful meditation before, but I really feel the difference which amazes me.’
Other SPs experienced a sense of joy, happiness, playfulness, creativity and imagination by participating in the storytelling activity:
‘Everybody is telling happy stories rather than sad stories. And I think in these times it just means so much. … I do like the idea of people having happy memories or happy incidents and whenever the discussions seem to trigger these moments in these stories and I think its upbeat, refreshing, and optimistic. Even if I can’t relate to it all, I sort of enjoy that scenario and the smiles that seem to come and yes, I think it’s very important. We need to smile at these times.’
Although one SP valued the meetings, they did question whether the activities and associated benefits were applicable to future SP work.
‘… the ease of discussing things with people. … I guess you get used to sort of connecting online. That part is good … but I’m not sure if … the stories that we talk about are necessarily going to be related to what we’re doing in [the SP programme].’
Most SPs expressed that the meetings enhanced their SP skills and competencies. They described how the meeting activities taught them how to be in the moment, focus, respond and react, and remain open to experiences, as aligned with SP methodology. The SPs identified that their heightened awareness of self and others contributed to the development or enhancement of these skills:
‘It’s creating more cohesion than we had before. … when it comes time to work together, I would be very surprised if we were not sort of in tune with each other a lot better.’
‘I think … it keeps a connection to what we do when we get back to doing videos and so on…. It just keeps a little tie to … what we’re doing … it just keeps you thinking about it and we are remembering how we used to do things.’
The SPs further acknowledged that the meeting activities deepened their ‘active listening’ skills and ‘empathy’, which ‘are important things if you’re going to play a role’. By processing information at a deeper level and spontaneously responding to others, the SPs explained that they felt better equipped to tackle various scenarios in their work:
‘… the big thing is the listening because when we’re doing our scenarios that’s really important you know. The listening part is a big part of it because the way that you respond to somebody else depends on how well you’ve been listening.’
The SPs recognized and appreciated the inherent structure of the meetings, including the regularity and format of the weekly sessions. They particularly valued the facilitation framework, noting that the facilitators clearly communicated expectations for each meeting, much as would be done for an in-person simulation session.
‘We’re told in advance what is going to happen, what we’re to think about and this is what we do with our [SP] sessions.’
They recognized and respected the importance of preparation for each meeting.
‘… you have to prepare before you come on and I have to think about what I’m going to, you know, whatever the topic.’
One SP clearly saw the link between the preparation for this meeting to the in-person work done before COVID-19:
‘… you always prepare us for our role in [the programme] … you’re given a scenario and then you have to think about it and how do I respond, … so it eases some of the stress and eases our way into thinking about communicating with people especially listening to people.’
The SPs also recognized the value of specifying the parameters for each activity. For example, by specifying the topic for the storytelling activity, the SPs felt empowered to challenge themselves in their work. They expressed that this sense of structure fostered a supportive environment, which promoted creativity and a sense of focus in their work:
‘I think it’s great, I like the fact that we get the topic given to us every week. People just aren’t talking away about different things … we’re concentrating on one topic.’
Through this structure, the SPs experienced a sense of relaxation:
‘It does seem to be a relaxed group and I think the weekly sessions has helped cultivate that; that people can be much more relaxed and show their true selves and share that with the group.’
Even in cases where specific meeting activities did not resonate with some SPs, they still commented on how the structured facilitation enhanced their overall programme experience:
‘Sometimes it gets boring … and I think it is reasonably well managed by [facilitators CS and LS] to control that. So, all in all … it’s been good.’
The aim of this study was to evaluate how older SPs think that their participation in regular structured 1-hour virtual meetings affects their well-being and SP skill development. Research prior to COVID-19 points out the devastating effect on older adults of loneliness, ‘a negative feeling resulting from a perceived deficit in companionship, quantity or quality in one’s relationships with … a community’ [23 p1]. Social distancing related to pandemic precautions has exacerbated this feeling and there have been many damaging effects on the health and wellness of older adults [27–29]. The perspectives of the older SPs presented in this study illustrate how a relatively straightforward, low-resource activity, combining effective practices in simulation and working with older adults, can offer an alternative to the harmful effects of social isolation in older adults, as well as promote the development of their skills as SPs.
The first theme, fostering meaningful and cohesive group connections, confirms research about counteracting the effects of COVID-19 on older adults through creating opportunities for ‘social connectedness … a positive, subjective evaluation of the extent to which one has meaningful, close and constructive relationships with other individuals, groups or society’ [23 p2]. It was clear that the SPs’ getting ‘to know their partners’ (i.e. fellow group members) has been essential to establishing a deeper sense of comfort and trust amongst them and with the programme facilitators. One of the silver linings of this situation is that, prior to COVID-19, the group did not get together in-person on a regular basis. Research indicates that older SPs desire more contact with SP programmes and can become distressed if this contact is not regular [8,9]; COVID-19 has provided this opportunity. The SPs have identified that they want to keep going indefinitely, as long as social distancing measures are in place, and even beyond. This deeper bond might never have been developed had it not been for COVID-19 restrictions. Research on older adult volunteers and older SPs also underscores that social connection is a strong motivator for the involvement of older volunteer SPs [8,9,30].
Gaining personal benefits, the second theme, including enjoyment, having fun and learning new things, has been highlighted in research as a strong driver for the participation of older SPs [8, 9]. Strategies to mitigate social isolation and loneliness, such as mindfulness, structured storytelling, reminiscence and technology use [20,21,23] were viewed with great favour by the SPs. Many of these strategies were new to the participants and, besides seeing how these activities could apply to their work as SPs, they were also able to apply some of the lessons learned to other aspects of their lives as well (e.g. to relax). Technology is sometimes identified as a barrier for participation of older adults [31] and initial group comfort level with technology ranged from very uncomfortable to comfortable using a computer, tablet or smartphone. However, the SPs enjoyed the challenge of adapting to new ways of doing things via technology. Despite some occasional technology glitches, all are able to fully participate virtually better than before COVID-19. Indeed, we have leveraged their skill development connecting virtually and have started online simulations, which they are embracing with competence and confidence.
The third theme highlights the SPs’ recognition and understanding that they are learning transferable skills and competencies for their SP work [32–34]. Active listening, empathy and being in the moment were repeatedly identified as being developed and strengthened. They appreciated that these meetings allowed them to work on their skills and keep them ‘fresh’, highlighting that potential cognitive decline when working with older adults should be monitored for and, if possible, mitigated through frequent opportunities for practice.
The fourth theme, appreciating structure, underscores the older SPs’ recognition of the framework we have in place that addresses their needs before, during and after simulation activities [12]. Activity topics are carefully chosen to stimulate storytelling and facilitate discussion. For the most part, topics are generic; for example, ‘What is your favourite food?’. However, this reminiscence can lead to emotionally laden recollections. Regardless, the SPs feel comfortable enough to share intimate and sometimes sad memories in this safe environment.
Furthermore, the older SPs recognized the crucial role of trained facilitators in guiding the meetings in a manner that made them feel comfortable and that built trust within the group. This finding highlights the importance of a skilled facilitator’s ability in a simulation environment to establish psychological safety, ‘the perception that it is safe to take interpersonal risks and that one will not be embarrassed, rejected or otherwise punished for speaking their mind, not knowing or asking questions’ [35 p1]. There is also an increasing recognition of the ethical imperative involved in ensuring the safety of all human beings who participate in a simulation, including SPs, and, by extension, unique groups of SPs, such as older SPs.[12,13,36,37]. Turner et al [38] note that ‘ a supportive facilitator is one who is inclusive, empowering, and encourages learner participation’ (p.5). Other qualities include flexibility, adaptability, honesty, displaying a respectful attitude, guiding the encounter in a way that aligns with the objectives of the session, being prepared and having a structured approach [35,38,39] Figure 2 – Facilitator tasks, skills and rationale – provides specific examples of facilitation tasks, facilitator skills required and rationale based on considerations when working with older adults [12].

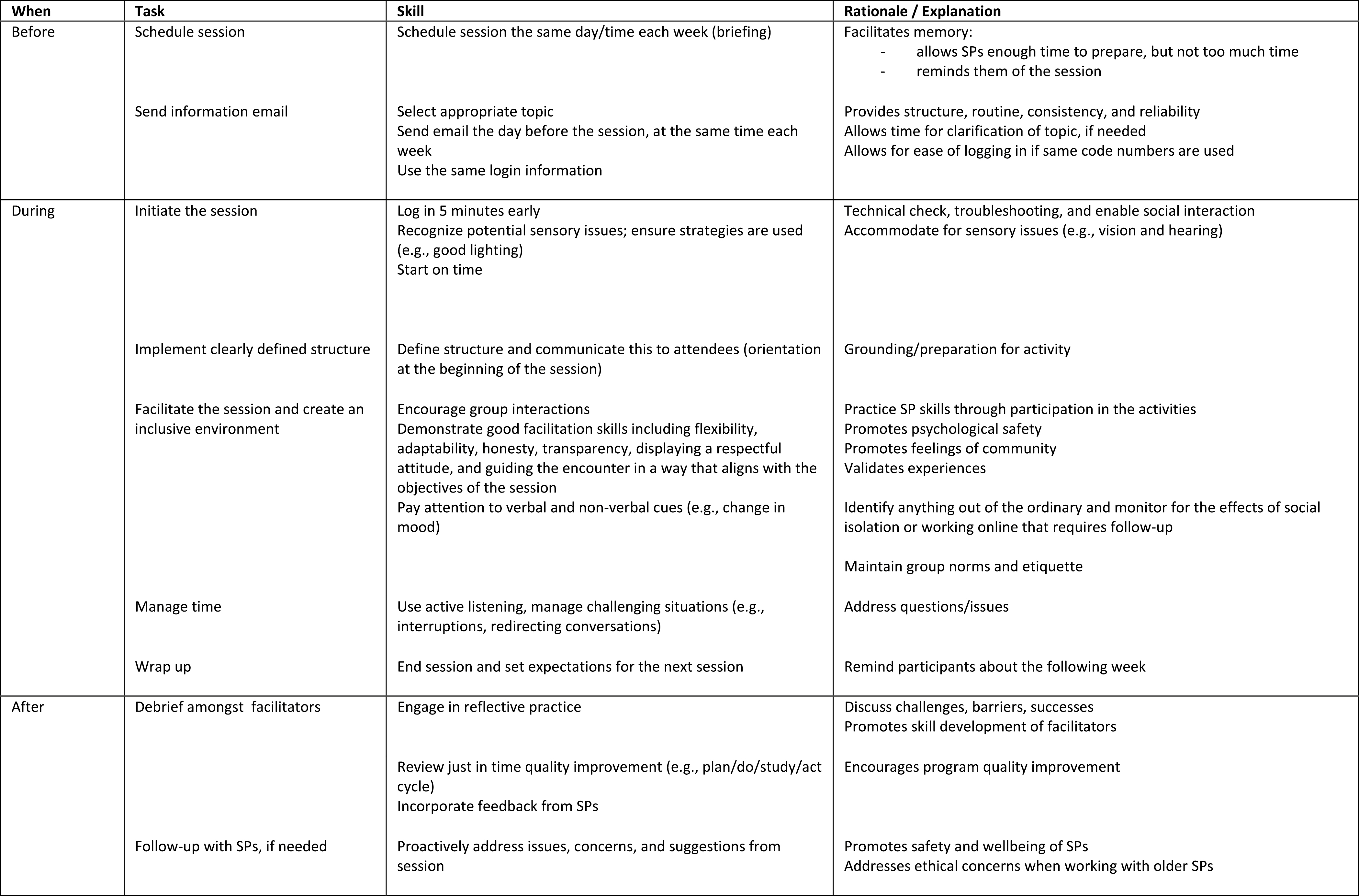
Facilitator tasks, skills and rationale
For this project, there were two facilitators. Cheung et al [40] note that while there can be challenges that arise with co-facilitating, often related to a lack of planning and communication, there can also be great advantages related to complementing each other’s approach, offering differing perspectives, supporting each other and cross monitoring and managing the expectations of participants. The co-facilitators for this activity have worked together in this SP programme for many years in face-to-face settings and had a shared mental model and a clear plan for proceeding through the meetings. They took turns leading the meetings and then stepping back to troubleshoot any technical issues and observe the older SPs to ensure their engagement and wellness. Regular debriefing after these meetings by the two facilitators has helped to clarify and improve skills and processes, and ensured follow up with SPs, if necessary, such as when SPs were unusually quiet or appeared distressed. So, for these meetings, co-facilitation, although more resource intensive, was beneficial on many levels and strengthened the effectiveness and safety of the interaction.
That this meeting is done online highlights the need for additional facilitation skills in this virtual environment, including managing the process and any challenging behaviours such as interruptions, and being aware of body language and facial expression on camera [41]. As SP work pivots increasingly towards this virtual environment [42,43], considerations for educators who facilitate online sessions with SPs, including the specific needs of unique populations of SPs, could be the subject for further research.
There are some limitations to this study. There may be a perceived conflict of interest or bias, as a group facilitator (LS) recruited participants and the other facilitator (CS) collected data from the very SPs with whom they work. However, it was clear from the data that the SPs and facilitators have a trusting relationship and strong rapport. To help ensure that the analysis remained true to the data, a qualitative researcher not connected to the programme or participants (CG) was involved in data coding and analysis. Another limitation may be access to equipment, internet connections, comfort with technology and accessibility issues (e.g. related to hearing loss). These limitations were mitigated with effective facilitation strategies, creating a space where SPs could share any challenges they were facing in their participation and, wherever possible, proactively seeking solutions (e.g. borrowing a tablet to replace a poorly functioning device).
Taken altogether, a structured, regularly occurring, virtual meeting is beneficial to the building and maintenance of SP skills for older adults, as well as their mental health and well-being. This approach could be applied to many other contexts and groups of SPs who are socially isolated or involved in distributed programmes where regular, in-person contact is not feasible with the proviso that a framework is in place featuring the basic tenets of effective simulation pre, during, and post simulation and there are skilled facilitators.
The authors wish to express their gratitude to the following individuals: The Baycrest SPs, Janis Sternhill, Tehila Tewel, Camille Silverio, Rosanne Aleong, David Conn, Brittany Ellington, Bev Kramer and other members of the Baycrest Centre for Education. Special thanks to Faith Boutcher and Rosalind Sham who reviewed an earlier version of this manuscript.
All authors contributed to the analysis of data, and to the conception, design and writing of the manuscript. All authors reviewed and approved the final manuscript.
Centre for Education, Division of Training and Simulation, Baycrest.
Available upon request within the parameters of the research ethics board approval.
Baycrest REB #16-04.
None.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.