
William Osler was the first to be credited with taking medical students out of the lecture theatre and to the bedside [1]. However, the COVID-19 pandemic has not just taken medical students out of lectures but also away from the bedside. Virtual reality simulation (VRS) can provide students with a computer-generated environment where users interact with virtual surroundings and patients in any location [2]. To mitigate the gap in clinical experiences we created an education package using VRS for medical students during the initial phases of the pandemic.
Could VRS provide a meaningful learning opportunity during the first wave? Could we elicit the strengths and weaknesses of virtual simulation in medical learning?
We used the Oxford Medical Simulation (oxfordmedicalsimulation.com) VRS platform where the learner manages an acutely unwell patient with specified learning objectives (opting for the 2-D to make it accessible to students at home). Scenarios were grouped, accompanied by didactic learning resources and released on a weekly schedule. Data were collected with consent on the number of scenarios accessed, performance score and student feedback.
The VRS course ran for 5 weeks (access extended to 11 weeks). In total, 224 students expressed an interest in accessing the VRS platform. Of the 224 students, 64 accessed the scenarios (50% first-year students). The students accessed 821 scenarios. The average score on all first attempts of scenarios was 75%; second attempts 78% and third attempts 90% (Figure 1). Qualitative feedback: ‘I like…the ‘real’ feel of talking to the patient, informing next of kin….it surprised me how real my patient feels’. ‘They are incredibly useful. … I much prefer doing them on a computer screen than in 3D. It does make for a different way of revising’.

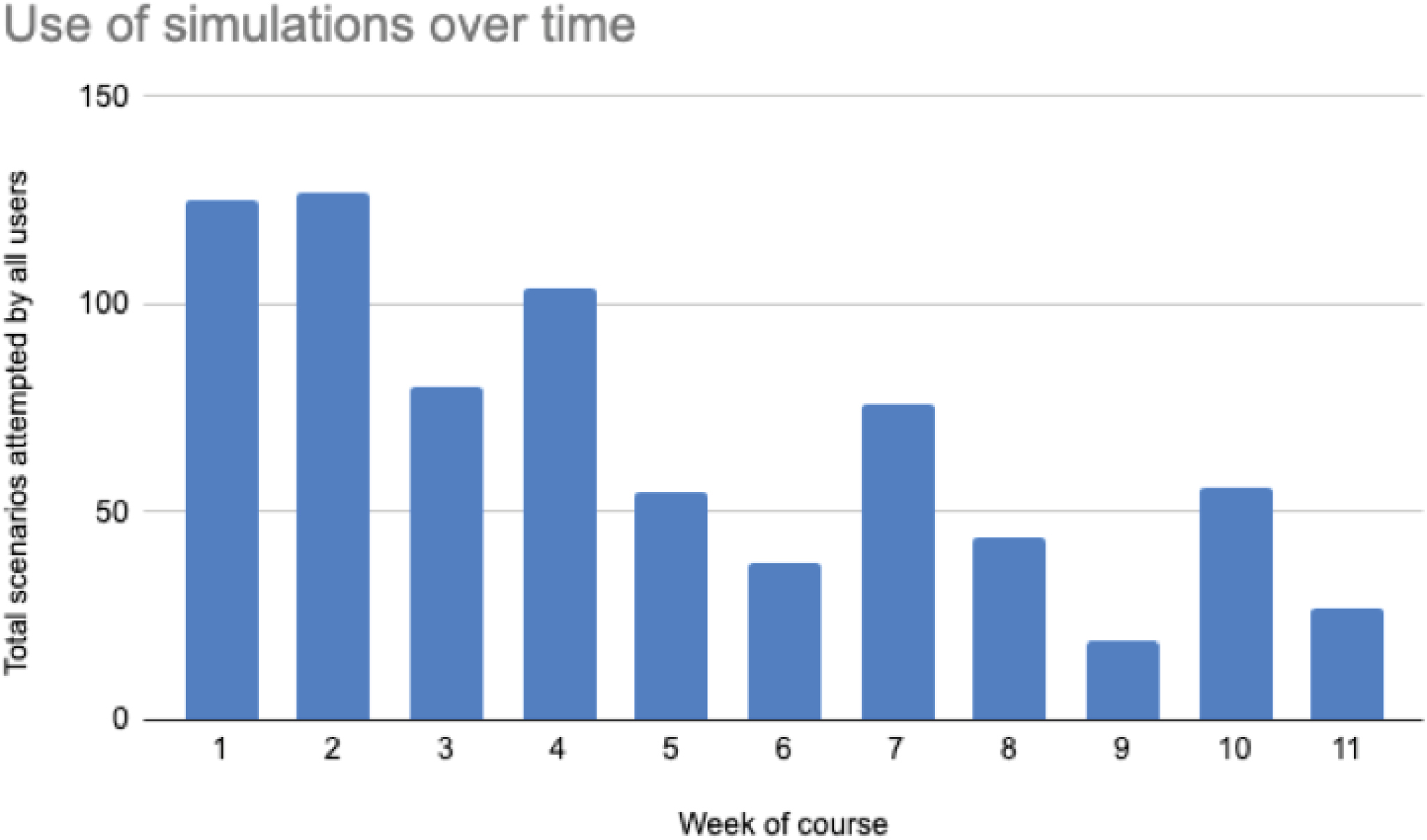
The high initial response rate suggested student interest and engagement. The low (21%) conversion rate to accessing the VRS platform may be explained by initial technical issues and the voluntary nature of the project. The quantitative data show the importance of repetition in improving learning. Participation over time may improve with incorporation into the medical school curriculum. Lower usage among the final-year medical students may be explained by volunteering and early commencement of clinical duties. This innovation reveals some strengths of VRS: basic equipment; learner-directed; improved performance and student interest. Overall, the VRS platform allowed the delivery of a rapid response to fill a gap in clinical education. The next phase of this project will be to provide live tutor-supported debrief.
2.