
The need for interprofessional education (IPE) has been recognized on the basis of compromised patient care due to ineffective communication and teamwork among healthcare providers. Using Simulation to enhance IPE has been advocated to achieve the competencies required for effective interprofessional collaborative practice. However, the implementation of this powerful tool and its integration into Indian medical education are a relatively recent development, gradually gaining momentum in recent years.
This study was undertaken to assess the attitudes and perceptions of a group of Indian medical and nursing undergraduates and faculty towards simulation-enhanced interprofessional education (Sim-IPE) before introducing this module at the institute.
A descriptive correlational design was conducted using the KidSIMTM ATTITUDES scale on a convenient sample of 82 students and faculty of medical and nursing colleges.
The total scores for the 30-item questionnaire revealed an overall positive attitude towards IPE and Simulation as a learning modality. Analysis of variance tests revealed lesser scores for students when compared to faculty.
A positive attitude towards Sim-IPE by students and faculty is promising, and it is the first step towards integrating Sim-IPE into the undergraduate curriculum in India.
The need for interprofessional education (IPE) is increasingly recognized and promoted by professional, accrediting and certifying bodies. The patient safety community advocates IPE as a mechanism to achieve the competencies required for effective interprofessional collaborative practice and healthcare simulation is evolving as a natural educational platform globally [1].
While physicians and nurses receive training in separate educational programmes, their coordination is essential in delivering effective and comprehensive patient care. In India, although the Competency-Based Medical Education curriculum, which has been introduced recently, includes elements of teamwork and collaboration, the medical and nursing curriculum does not explicitly include interprofessional team training. Teamwork training, including IPE competencies conducted using simulation and debriefing, is leading to improved patient care [2]. The first step towards integrating a Simulation-enhanced interprofessional education (Sim-IPE) module into the undergraduate curriculum is to assess the attitude and perception of the undergraduates and faculty towards Sim-IPE. This study was undertaken to explore the perceptions and attitudes of students and faculty of a tertiary care hospital in South India towards IPE, simulation as a learning modality and teamwork concepts.
A descriptive correlational design was conducted using an online questionnaire on a convenient sample of a total of 82 students and faculty of medical and nursing colleges of the institute. The students included were final-year medical and nursing interns and the faculties were teachers engaged during the intern years. The minimum sample size was calculated as 78 considering this population using RaosoftR software with a confidence level of 95%, a margin of error of 10% and a response distribution of 50%. The survey was mailed to the target population and responses accepted until it crossed the threshold of 80.
The study was conducted at a tertiary care hospital in South India. The participants included undergraduate interns and faculty of the medical and nursing college. The invitation to participate included information about participation and consent, clearly stating that participation was voluntary and confidential. The study protocol received approval by the Institute’s Ethics and Research Committee (Protocol number 419/18).
A self-administered questionnaire was used for data collection. The questionnaire was sent online to the participants as a Google form during the month of September 2018. The KidSIMTM Attitude Towards Teamwork in Training Undergoing Designed Educational Simulation (ATTITUDES) questionnaire [3] was used as the research tool to collect data for the purpose of this study. Other data collected included whether the participant was a medical or nursing student or medical or nursing faculty. No other demographic details were collected.
The KidSIMTM ATTITUDES questionnaire was developed by Sigalet et al. [3]. It is a 30-item questionnaire developed as a standardized measure to assess student perceptions of and attitudes towards educational simulation and the use of simulation as a learning modality. The scale was developed using concepts taken from literature and pre-existing scales. Factor analysis was conducted to examine the psychometric properties and to assess the construct validity of the scale. The analysis of the instrument carried out by the authors supported the presence of five sub scales: The five subscales of the questionnaire include Relevance of Simulation (six items), Opportunities for IPE (seven items), Communication (eight), Roles and Responsibilities (six items), Situational Awareness (three items). The scale was reported to have a high level of internal consistency reliability (Cronbach’s alpha was 0.95). The scale is a Likert-type scale with options that range from 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree and 5 = strongly agree, producing a range score between 30 and 150.
Statistical Package for the Social Sciences Version 22.0 was used to analyse the data. The data were analyaed using paired t-test to compare mean scores and one-way analysis of variance (ANOVA) test. Significant differences between the groups were analysed using Tukey’s post hoc test. The results were considered to be statistically significant – p < 0.05.
The response rate was 82% out of the total population of undergraduate interns and faculty coordinators with 74.4% female (n = 61). Participants were medical faculty (n = 23), nursing faculty (n = 18), medical intern (n = 26) and nursing intern (n = 15). The total participants were composed of 50% faculty (n = 41) and 50% students (n = 41).
In the sample (n = 82), 47.6% of the participants (n = 39) had experienced Simulation-based education but none had prior experience in Simulation-based IPE. All participants (n = 82) reported previous team-based learning. While 22% of them (n = 18) acquired this team-based experience through courses, 14.6% (n = 12) from work experience and 13.4% (n = 11) from workshops. Others comprised the remaining 50% (n = 41) who reported having acquired experience from combined sessions which included courses, seminars, workshops and work experience. Out of the sample of 82 participants, 56.1% had not participated in any Communication skill training programme. Demographic data are described in Table 1.

| Variable | Frequency (N) | Per cent (%) |
|---|---|---|
| Gender | ||
| Female | 61 | 74.4 |
| Male | 21 | 25.6 |
| Participant | ||
| Faculty | 41 | 50 |
| Medical faculty | 23 | 28.04 |
| Nursing faculty | 18 | 21.96 |
| Undergraduate | 41 | 50 |
| Medical intern | 26 | 31.7 |
| Nursing intern | 15 | 18.3 |
| Prior simulation experience | ||
| No | 43 | 52.4 |
| Yes | 39 | 47.6 |
| Prior team-based learning | ||
| Yes | 82 | 100 |
| No | 0 | 0 |
| Type of teamwork experience | ||
| Courses | 18 | 22 |
| Workshops | 11 | 13.4 |
| Work experience | 12 | 14.6 |
| Others (combined) | 41 | 50 |
| Communication skills training | ||
| No | 46 | 56.1 |
| Yes | 36 | 43.9 |
Bold numbers are to depict the total.
The data collected using the KidSIMTM ATTITUDES questionnaire (with a total range of 30–150) were promising with a mean total score of 128.68 (SD = 17.09). Of the entire sample, only one medical student reported an attitude that fell in the minimum scale range of 30. The means of the five subscales were well above the possible mean scores of each of those subscales as depicted in Table 2.

| Subscale | Number of items | Subscale potential range | Subscale potential mean | Mean (SD) | Median |
|---|---|---|---|---|---|
| Relevance of Simulation | 6 | 6–30 | 18 | 25.68 (3.6) | 26 |
| Opportunities of IPE | 7 | 7–35 | 21 | 29.56 (4.2) | 29 |
| Communication | 8 | 8–40 | 24 | 35.15 (4.9) | 35 |
| Roles and responsibilities | 6 | 6–30 | 18 | 25.65 (3.6) | 25 |
| Situational awareness | 3 | 3–15 | 9 | 12.65 (1.8) | 12 |
One-way ANOVA with Tukey’s post hoc test was applied to compare the total attitudes scores between the groups as shown in Table 3. Table 4 shows the comparison for the variable related to simulation. With regards to one of the subscales, namely, ‘Relevance of Simulation’, there was a statistically significant difference in mean scores among the groups with higher scores in the Faculty group when compared to the Student group. Figure 1 depicts the mean scores of the groups.

| Participants | N | Mean | Standard deviation | Minimum | Maximum | ANOVA | |
|---|---|---|---|---|---|---|---|
| F value | p-Value | ||||||
| Medical faculty | 23 | 134.0870 | 11.33744 | 112.00 | 150.00 | ||
| Nursing faculty | 18 | 136.9444 | 10.42888 | 118.00 | 150.00 | 4.842 | 0.004 |
| Medical intern | 26 | 122.0769 | 21.84110 | 30.00 | 150.00 | ||
| Nursing intern | 15 | 121.9333 | 15.49408 | 91.00 | 143.00 | ||
| Total | 82 | 128.6829 | 17.09875 | 30.00 | 150.00 | ||

| Dependent variable | (I) GRP | (J) GRP | Mean difference (I–J) | Standard error | p-Value |
|---|---|---|---|---|---|
| Simulation | Faculty medical | Faculty nursing | −0.46860 | 1.07169 | 1.000 |
| Student medical | 2.93311* | 0.97482 | 0.021 | ||
| Student nursing | 3.15362* | 1.13021 | 0.040 | ||
| Faculty nursing | Faculty medical | 0.46860 | 1.07169 | 1.000 | |
| Student medical | 3.40171* | 1.04420 | 0.010 | ||
| Student nursing | 3.62222* | 1.19057 | 0.019 | ||
| Student medical | Faculty medical | −2.93311* | 0.97482 | 0.021 | |
| Faculty nursing | −3.40171* | 1.04420 | 0.010 | ||
| Student nursing | 0.22051 | 1.10417 | 1.000 | ||
| Student nursing | Faculty medical | −3.15362* | 1.13021 | 0.040 | |
| Faculty nursing | −3.62222* | 1.19057 | 0.019 | ||
| Student medical | −0.22051 | 1.10417 | 1.000 |
*p-Value < 0.05 is significant.

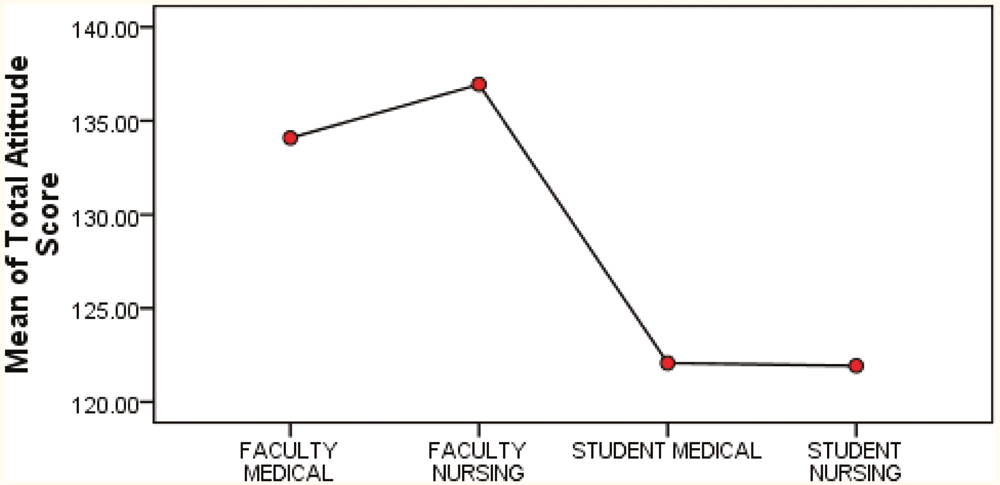
Mean scores of attitudes and perceptions among participants
An extensive literature review yielded few data from India pertaining to the implementation of a Sim-IPE programme on teamwork. The system of medical and nursing education in India is currently focussing on incorporating learner-centric and holistic approaches to teaching. These approaches go beyond didactic teaching and aim to develop well-rounded and confident healthcare professionals. Indian students are now increasingly being exposed to teaching methodologies that focus not only on technical and clinical acumen, but also, soft skills such as leadership, communication, professionalism, empathy and ethical decision-making. The National Medical Commission has also introduced an AETCOM (Attitudes, Ethics and Communication) module and has mandated skills training using simulation for undergraduate medical students. Thus, leading institutions are adopting simulation and paving the way for others [4].
There has been considerable progress in simulation-based training and education in India in the past 10 years. IPE is one such method of collaborative learning that encourages better communication and teamwork among healthcare providers. A study introduced for medical and midwifery students in a secondary-level hospital in India attempted to evaluate the feasibility and benefit of an interprofessional skills training workshop. Both groups found the workshop improved their confidence in performing vaginal examinations and births. The main themes which emerged were ‘getting hands-on’ experience, learning by simulation, valuing interprofessional experience and ensuring equal learning opportunities for all professional groups [5]. Kumar et al. conducted mobile interprofessional obstetric and neonatal workshops for medical and midwifery staff and students across three locations in India. The primary takeaways were acquiring expertise in knowledge and procedural skills, developing non-technical skills, adopting a methodical approach to managing obstetric and neonatal emergencies, and engaging in team-based learning facilitated by simulation [6].
This is promising but to sustain such interprofessional modules, they need to be integrated as Sim-IPE in undergraduate curricula. Educators in the healthcare professions, need to understand student and faculty attitudes towards the use of IPE so that they can align and adapt curricular objectives to meet the needs and intended learning outcomes. A cross-sectional survey conducted in South India by Mohammed et al. assessed the attitude of dental students towards IPE using Readiness for Interprofessional Learning Scale (RIPLS) and discerned a mostly positive and encouraging attitude towards interprofessional learning [7].
When the motivation for simulation as a learning modality is understood, that understanding provides evidence and guidance for the delivery of an interprofessional team training curriculum [3]. In this study, we assessed the attitudes and perceptions of students and faculty toward Sim-IPE using the KidSIMTM ATTITUDES questionnaire. The majority of participants showed a high level of understanding and optimism about simulation, IPE and teamwork concepts inclusive of roles and responsibilities, communication, and situation awareness, where their scores were encouraging on all five subscales that composed the ATTITUDES questionnaire. There were no previous studies in India that assessed the perception of students and faculty towards Sim-IPE and teamwork using this questionnaire. A similar study was conducted in Jordan on nursing students with a translated version of this questionnaire [8]. The total attitude score recorded by the participants in the Jordanian study (mean total score of 131.2 ± 14.4) was similar to the results seen in our study (mean total score of 128.6 ± 17.0). That study was conducted only with nursing students. The current study included both medical and nursing students. We also assessed the perception of the faculty of both professions. In this study, the attitudes and perceptions were higher among faculty when compared to students, possibly due to their previous experience with activities involving simulation and teamwork. The findings of the current study were similar to those of Sigalet et al. [3] who found that the use of team-based learning improved perceptions of and attitudes towards simulation-based curriculum. Other scales available for assessing the attitudes towards IPE are ‘Readiness for Interprofessional Learning Scale’ and the ‘Interdisciplinary Education Perception Scale’, but they do not cover the domain of Simulation as a learning approach for IPE. A study conducted in Malaysia explored the two scales (RIPLS and IEPS) and their psychometric properties on students from four different professions and they revealed that both these scales have their own ability to detect differences in students’ attitudes towards IPE in their own way [9].
Although the results obtained were promising, the sample size and single sample site are limiting factors; therefore, the results are extrapolated on with caution. Moreover, the chosen sampling method may not provide results that can be generalized to a broader population. Focus group interviews would have helped in further exploring the recorded attitudes and perception scores.
This study provides insight into mechanisms that might be used to develop appropriate objectives for learners, and help in outlining future Sim-IPE modules. It is suggested that implementing these modules at a time when the participants’ perceptions of and attitudes to simulation are well established, can help to improve the outcomes of this educational strategy.
None declared.
None declared.
None declared.
None declared.
Ethics clearance obtained from IRB and consent obtained for participation.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.