
Virtual reality (VR) simulation is a rapidly expanding disruptive technology within healthcare professions education with the possibility of significantly transforming how healthcare education is delivered. There is a perceived gap in the current synthesized literature of how VR is being used to teach and assess key skills relating to situational awareness (SA) and decision-making (DM) across the spectrum of undergraduate healthcare professions. This paper details the scoping review protocol that will address this current gap.
The scoping review will examine ‘What is known about the use of VR within simulation training for SA and DM behavioural skills in healthcare professions education?’. This main question will be addressed by synthesizing the answers to three sub-questions: (1) In what contexts is VR used within simulation training for SA and DM behavioural skills in healthcare professions education? (2) What outcome measures are used to examine the impacts of VR use within simulation training for SA and DM behavioural skills in healthcare professions education? (3) What educational theories underpin VR use within simulation training for behavioural skills in healthcare professions education?
Nine databases, PubMed, PsychINFO, Embase, Scopus, Web of Science, CINAHL, ERIC, and Google Scholar, will be searched using a pre-defined search strategy with explicit inclusion and exclusion criteria. A data extraction template will be used to map out the data before summarizing, synthesis and reporting.
This scoping review aims to address the current gap in the literature regarding what is known about VR simulation and DM and SA across undergraduate health education programmes, identifying current trends and uses as well as gaps in the published literature for further exploration.
Virtual reality (VR) simulation is a rapidly developing area of simulation-based practice within undergraduate healthcare education curricula with the opportunity to transform how healthcare education is delivered [1]. Coupled with the increased use in teaching, there has been an associated expansion of published research within the healthcare education literature relating to VR use in simulation [2]. With increasing student numbers across the healthcare disciplines and the need to find alternatives to, or ways to complement, clinical placement learning, VR offers the opportunity for us to consider how teaching may be delivered differently [3].
VR is defined by the Society of Simulation in Healthcare as ‘The use of computer technology to create an interactive three-dimensional world in which the objects have a sense of spatial presence; virtual environment and virtual world are synonyms for virtual reality’ [4]. VR environments are often described based on the technology being used, for example, head-mounted display (HMD-VR) or other technologies such as computer-based VR environments controlled by mouse, keyboard, voice or haptic devices[4,5].
Further developments in VR have led to additional definitions that are currently being used within the healthcare education landscape including augmented reality (AR), a hybrid form of VR, whereby there is a virtual overlay of the world but with no real-world physical interaction [4], and mixed reality (MR), a digital overlay on items or locations that can be interacted with. MR often encompasses the definition of AR but has more interactive features than typical AR [4,6].
The blend of what is physically present to what is 100% computer generated is expressed in this continuum: Reality – AR – MR – VR [4]. (See also Hsieh and Lee for further information on VR and AR applications in medical and healthcare education [7].)
The increasing interest in VR use within healthcare and healthcare education has resulted in a plethora of varying definitions. In their recent review, Abbas et al. found that in the last 5 years, 58 articles were published offering definitions of VR, whereas in the previous 15 years, there had only been 30 in total [2]. In this study, we will use the definition of VR as proposed by Abbas et al.: ‘VR is a three-dimensional computer-generated simulated environment, which attempts to replicate real world or imaginary environments and interactions, thereby supporting work, education, recreation, and health’ [2]. The principles within this definition, of a three-dimensional computer-generated simulation of reality to support education, will be taken to refer to all the extended realities as well as patients represented in virtual environments with participants interacting with the patient and wider environment for the purpose of this review [5].
A recent scoping review identified that for medical students alone, VR has been used for teaching 3D anatomy visualization, surgical technical skills, communication skills and empathy [8]. The integration of extended realities within the curricula for the delivery of clinical teaching and experiential learning has sparked an increased academic interest in the topic [1]. These extended reality technologies offer healthcare educators a potential solution to address some of the difficulties in the resource-intensive delivery of healthcare simulation, making delivery more flexible in terms of both place and time. One potential area where VR simulation may be beneficial is in teaching and assessing situational awareness (SA) and decision-making (DM), important closely related and interdependent cognitive behavioural skills for current and future healthcare professionals [9]. In this review, we will use the term ‘behavioural skills’ instead of the more traditional term ‘non-technical skills’ as this better reflects modern understanding of both simulation and real-world practice terminology [10,11].
DM is a ‘complex process of observation, information processing, critical thinking, evaluating evidence, applying knowledge, problem solving, reflection, judgement to select best option from available choices to optimize patients’ health and minimize potential harm’ [12], p7. Whilst SA is defined by Endsley as ‘the perception of the elements in the environment within a volume of time and space, the comprehension of their meaning, and the projection of their status in the near future’ [13], p34. Both SA and DM are intrinsically related concepts with SA informing DM [14,15].
There is a strong history of using simulation to expose learners to situations that are low occurrence and that otherwise, they would not be able to experience through traditional apprentice-style training. A recent review examined the teaching of SA in simulation-based education in general, focusing particularly on nursing students, but did not specifically focus on using VR techniques [16]. Other recent relevant reviews examined VR within medical student education without focusing on SA or DM, or VR within nursing student education for DM only [8,17].
Therefore, there is a current gap for a synthesis of the research on VR use in teaching and assessment of SA and DM in health professions education.
The aim of a scoping review is to determine the scope or coverage of a body of literature on a given topic and give an indication on the volume of studies available as well as an overview of the focus. They are useful for examining emerging evidence when it is unclear what other, more specific questions could be addressed in a systematic review, identify gaps in the literature or suggest whether new empirical research is required [18]. Scoping reviews enable researchers to consider and clarify complex concepts, particularly with respect to emerging disciplines where the numbers of studies available restrict the possibility of systematic reviews [19]. In this case, there is a need to clarify how VR technology is currently being used to train and assess SA and DM within health professions’ education and identify any gaps in the evidence base for its use. The scoping review of methodological framework developed by Arksey and O’Malley (Figure 1) will be applied in this review [20].

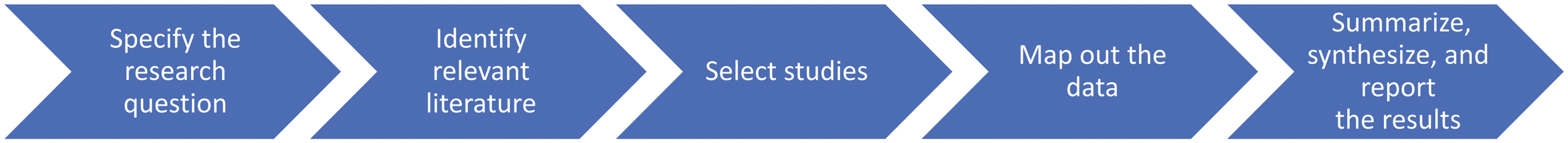
Scoping review framework.
Specifically, within this scoping review we will (1) specify the research question, (2) identify relevant literature, (3) select studies, (4) map out the data, (5) summarize, synthesize, and report the results. This manuscript outlines the protocol for this scoping review.
The main research question to be addressed by this scoping review is ‘What is known about the use of VR within simulation training for situational awareness (SA) and decision making (DM) non-technical skills in healthcare professions education?’ This main question will be addressed by synthesizing the answers to the following three sub-questions:
To answer the above research questions, we will undertake a scoping review as we seek to map existing research in this area and identify gaps in the current research [21].
To select the relevant literature for review, pre-defined eligibility criteria will be applied relating to participants, types of evidence, language and context.
Participants sampled within the evidence synthesized in this review must focus on undergraduate healthcare professions education in either the clinical workplace or education environments. Previous reviews have focussed on one healthcare professional group only [8,16] or predominantly postgraduate learners working in teams [22]. The undergraduate population is of particular interest as these learners have limited exposure and practice in this skill development, and increasing numbers of health professions students are putting significant pressure on healthcare systems already under strain [3]. This review will consider the spectrum of healthcare education as simulation becomes more integrated into a wider remit of undergraduate and interprofessional healthcare programmes. Undergraduate programmes are of particular interest as many of these behaviours and skills are considered to be learned in the workplace; however, there are limited opportunities for the systematic teaching of these behaviours to be explicitly taught and assessed in the clinical environment at the undergraduate level [23,24].
The scoping review will include any peer-reviewed empirical primary research studies, and published academic work of either quantitative or qualitative research study designs. The review will include experimental and non-experimental studies describing VR use. There will be no restriction by study quality as the primary focus of the scoping review is to understand the contexts VR is being used, the outcome measures of VR simulation in SA teaching and assessment, and what educational theories are underpinning VR use in this context. The reference lists of reviews will be screened for relevant primary studies that fall within the pre-defined inclusion criteria, and these will be charted within the scoping review. Reviews or opinion pieces will be excluded if they do not contain participants; however, reviews will be scrutinized for primary studies meeting the inclusion criteria. Descriptive reports, as long as there are participants will remain included.
Articles will be considered for inclusion if they focus on VR simulation for teaching or assessing SA or DM in undergraduate healthcare professions education. The context of any evidence can be within either the clinical workplace or any undergraduate education environment. Evidence will be included from any geographic region. Articles will be included if they meet the definition of VR (including AR and MR) as proposed by Abbas et al. [2] including all forms of VR delivery such as computer screen or HMD.
For practical reasons, evidence to be included in this review must be published in English and is felt unlikely to introduce significant bias [25].
The search strategy will use identified medical subject headings (MeSH) and keywords within the titles, abstracts and index terms used within published research. These will include:
We will also conduct a reference list search of review articles for additional studies [21]. See Supplemental File 1 for details of the search strategy.
Nine different database searches will be included:
Boolean operators such as truncations (*) will be used where appropriate.
After the searches have been conducted, all citations will be uploaded into the reference management database, Rayyan (www.rayyan.ai) and de-duplication will occur. Titles and abstracts will be screened by a first reviewer against specified inclusion and exclusion criteria (Table 1). Second, the remaining publications will be screened at full-text stage by at least two researchers, for inclusion. All three reviewers will contribute to this stage with one reviewer contributing to all screening and the other two reviewers sharing the second reviewer workload. Reasons for exclusion, at the full-text stage, will be recorded by the researchers. Disagreement regarding the inclusion of articles will be resolved by discussion in the presence of a third reviewer from the ‘conflict’ list produced by Rayyan. The screening process will be reported using the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for scoping review (PRISMA-ScR) diagram [29]. If full texts are unavailable through institutional policies, authors will be contacted directly. The reviewer team consists of CB – clinician and senior clinical lecturer in simulation, AL – director of healthcare education and innovation centre and MC – medical student. All reviewers have prior experience in academic literature review.

| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population | Population: Undergraduate healthcare professional students | Students on non-healthcare professions courses |
| Postgraduate healthcare workers | ||
| Intervention | Intervention: VR/AR/MR use either via head-mounted device (HMD) or using other devices such as computing virtual environments within simulation training | VR/AR/MR use not in simulation training |
| Outcome | Cognitive non-technical skills – Situational awareness or decision-making |
Data will be extracted from each included article using a data extraction template including variables recommended for reporting in simulation studies [30]. The terminology used will match the definitions in the Society of Simulation in Healthcare dictionary [4]. Extracted variables will include:
A pilot data extraction exercise will be conducted before starting the main extraction exercise.
Following extraction and charting, extracted data will be synthesized to answer the scoping review research questions. The number, type and location of studies will be presented numerically, where possible using tables. The various contexts VR is being used in both for teaching and assessing SA and DM will be presented descriptively with examples including coverage of the varying professional disciplines and individual contexts within the disciplines. Quantitative and qualitative data (where available) will be synthesized regarding impact measurements and tools used in assessing SA and DM. Our third sub-question regarding educational theories will be synthesized and presented descriptively. Where gaps in the literature are identified, these will be presented as guidance for future research work.
By adopting the scoping review framework outlined above, we will address the current gap in the literature regarding understanding the implementation of a rapidly accelerating simulation modality in assessing the teaching and assessment of SA and DM across the undergraduate healthcare education programmes. This will provide an overview of current use and identify gaps for future research.
See attached Supplemental File 1. Detailed search strategy.
CB conceived the initial idea for the study. CB, AL and MC devised the research protocol. CB wrote the initial manuscript. All authors contributed to the writing and editing of the manuscript.
MC was funded through a University of Aberdeen Student Project bursary.
Not applicable.
There are no conflicts of interest to report.
CB is a consultant in Emergency Medicine and an honorary senior clinical lecturer in clinical simulation at the University of Aberdeen.
AL is the director of the centre for healthcare education research and innovation (CHERI) at the University of Aberdeen.
MC is a medical student at the University of Aberdeen.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.