
High-fidelity simulation is embedded in all aspects of anaesthesiology training. Despite advances in manikin technology, significant limitations relating to ventilatory realism persist [1]. Psychological immersion – the participants’ perception that the simulation is an accurate reflection of a real-life scenario – impacts the participants’ learning experience [2]. A lack of feedback from the manikin regarding the adequacy of either spontaneous or assisted ventilation hampers psychological immersion. Our innovation delivers haptic and visual feedback to ensure a more immersive experience for our simulation participants.
In our adult tertiary hospital multidisciplinary in situ simulation-based education takes place on a weekly basis using a SimMan Essential (Laerdal, Norway). Scenarios are based on real-life cases and almost all of them involve active airway management. Standard high-fidelity manikins ‘breathe’; however, they do not actively inhale and exhale. Manikin chest rise and fall correspond to the respiratory rate set by the console operator.
During airway management, adequacy of ventilation is determined by a combination of physiological parameters (e.g. SpO2 , capnography), and mechanical parameters (e.g. chest rise and fall, filling and emptying of a Mapleson or ventilator reservoir bag that the patient is breathing from). In cases where the patient requires assisted ventilation (e.g. via face mask, supraglottic airway or tracheal tube) this reservoir bag provides additional important information about lung compliance and ease of ventilation during manual ventilation. Therefore, in real life, the emptying and filling of this reservoir bag provide crucial breath-by-breath haptic and visual feedback to the user about adequacy of patient ventilation [1,3]. Prior to the development of our system, simulation participants would have to be told whether or not the bag is moving or not moving as the scenario evolved, leading to multiple interjections by the facilitators and consequent loss of psychological immersion. Our innovation addresses this currently unmet need to provide realistic dynamic feedback when assessing spontaneously ventilating manikins or providing ventilatory assistance.
Our system aims to give the simulation participant haptic and visual feedback through conventionally used and easily obtainable anaesthetic breathing circuits.
The system is composed of the following parts:
1. Adult face mask x1
2. HME filter with port for capnography tubing x1
3. Capnography tubing x1
4. Mapleson circuit with APL valve (Armstrong Medical, Coleraine, Northern Ireland) x1
5. 22-mm anaesthetic breathing system 4m (Intersurgical, Berkshire, UK) x1
6. Luer elbow x2 (available as part of the Intersurgical (Berkshire, UK) 22-mm anaesthetic breathing system with 2-L bag, Luer elbow, monitoring line and limb 1.6 m)
7. Oxygen tubing x1
8. Air or oxygen cylinder x1
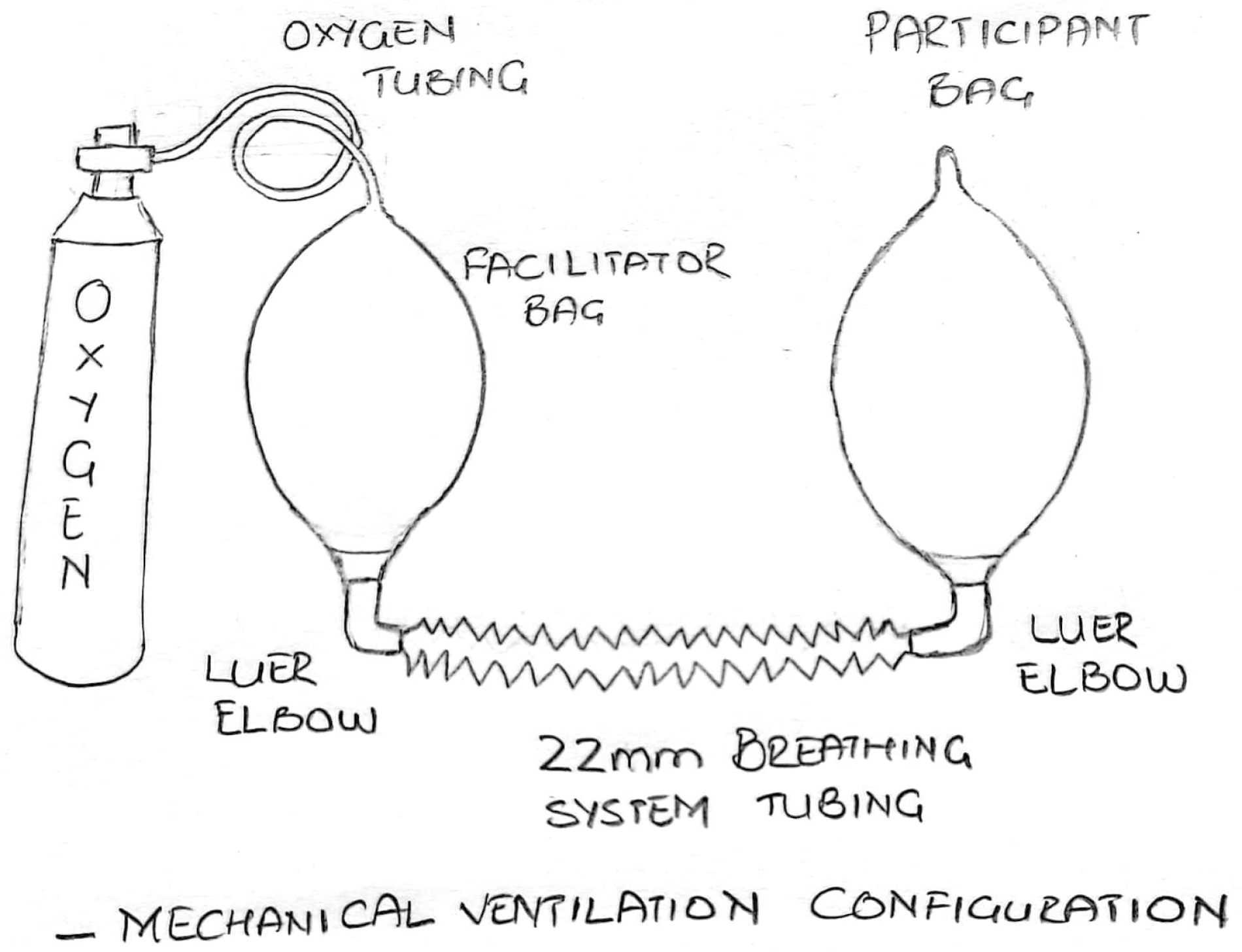
Figure 1 shows assembly of the components for a Mapleson circuit and Figure 2 demonstrates the set-up for the ventilator circuit (in this case for a Drager Aisys anaesthetic machine), respectively. Figure 3 and Figure 4 represent the schematic diagrams of the two configurations. The two possible configurations allow simulations to take place in environments with and without an anaesthetic machine.


Equipment assembly for the Mapelson circuit configuration


Equipment assembly for the mechanical ventilation configuration

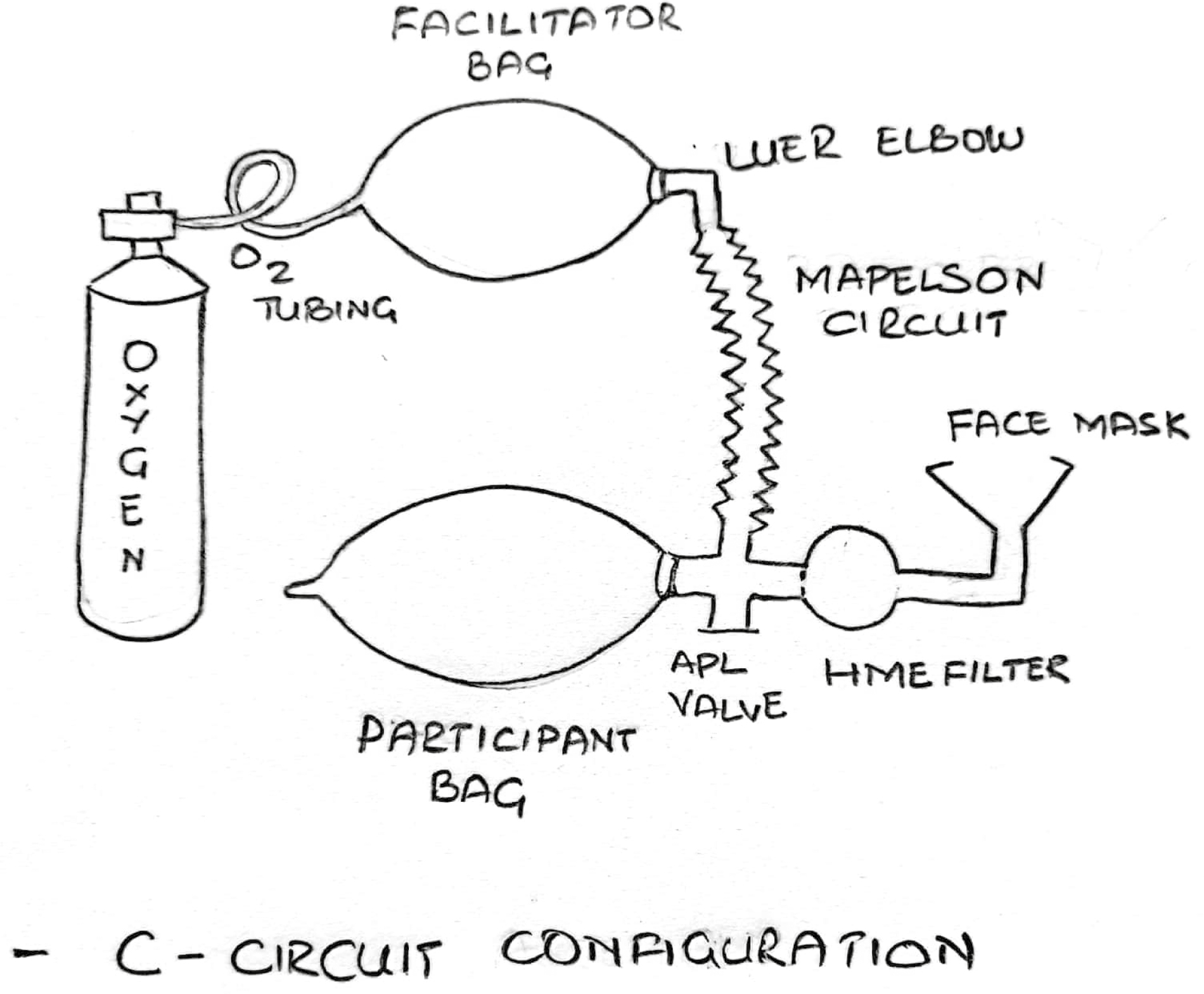
Schematic representation of the Mapelson circuit configuration
The reservoir bags and breathing circuit tubing form a closed system. No gas should exit the system via the face mask or the APL valve. To achieve this the APL valve and the APL valve limb that leads to the HME filter are occluded permanently (we used glue). The appearances of the APL valve are unchanged and the dial can still be opened or closed by the participant thereby ensuring realism is preserved. This closed system is filled via oxygen tubing connected to the facilitators’ reservoir bag. Once filled to the required tension the air cylinder is closed. Spontaneous respirations are mimicked by the facilitator squeezing the facilitator reservoir bag. This is visualized by the participant as the manikin bag moving. The participant can ventilate the manikin by squeezing their bag, which in turn refills through squeezing by the facilitator, if the manikin is being adequately ventilated. If the manikin is not being ventilated the pressure in the circuit can be reduced by momentarily breaking the circuit and letting out a small amount of gas. The bag will not refill in the characteristic manner that corresponds to adequate manual bag-mask ventilation. If the participant subsequently can ventilate the patient (e.g. after inserting a guedel or supraglottic airway), the system can be quickly re-pressurized again by opening the air cylinder. When the participant squeezes their bag, it will refill when the facilitator applies gentle pressure to their bag. Therefore, our system gives the facilitator full control over what visual and haptic feedback the participant receives as the scenario evolves. In simulations where the anaesthetic machine is used its ventilator circuit is separate to our system, so it can be used as normal by the participant which further enhances psychological immersion.
The system utilizes easily obtainable low-cost anaesthetic equipment. It is therefore ideal for use in low-resource settings [4].
This system is used at our weekly simulation sessions which are attended by approximately 12 anaesthesiology trainees (from a department of 36 anaesthesiology trainees, who range from beginning to near completion of their anaesthesiology training), two anaesthetic nurses and two recovery nurses. Participants attend on a rolling basis and therefore get significant exposure to simulation-based medical education. During the development phase informal interviews of participants and consultant anaesthesiologists in our department were carried out. Modifications to improve the system were made and all agreed that the system provided excellent dynamic feedback. In addition, we recently conducted an online survey of our anaesthesiology trainees. Most of the respondents were registrar level (73%) and all agreed that the system improves haptic and visual feedback.
Realistic haptic and visual cues from the manikin during airway management are crucial for participant buy-in and immersion. We are in the process of evaluating the system in other clinical settings (ICU, ED) where this feedback is paramount [5].

Schematic representation of the mechanical ventilation configuration
None declared.
None declared.
None declared.
None declared.
None declared.
1.
2.
3.
4.
5.