
Gender minorities experience extensive health inequities. Discrimination and bias in healthcare are contributing factors. Increasingly, medical educators are utilizing patient simulation to teach gender-affirming clinical skills. However, institutional practices vary widely in case authoring, casting and training. To date, no guidance for ethical practice has been established. Gender minority healthcare providers offer an important perspective on this due to their patient simulation experience and embodied knowledge.
Transgender and non-binary healthcare providers and trainees (n = 21) took part in semi-structured interviews that focused on their experiences with, and perceptions of, simulation and gender-affirming care. Participants were asked to consider several casting scenarios. Data were analysed using inductive thematic discourse analysis.
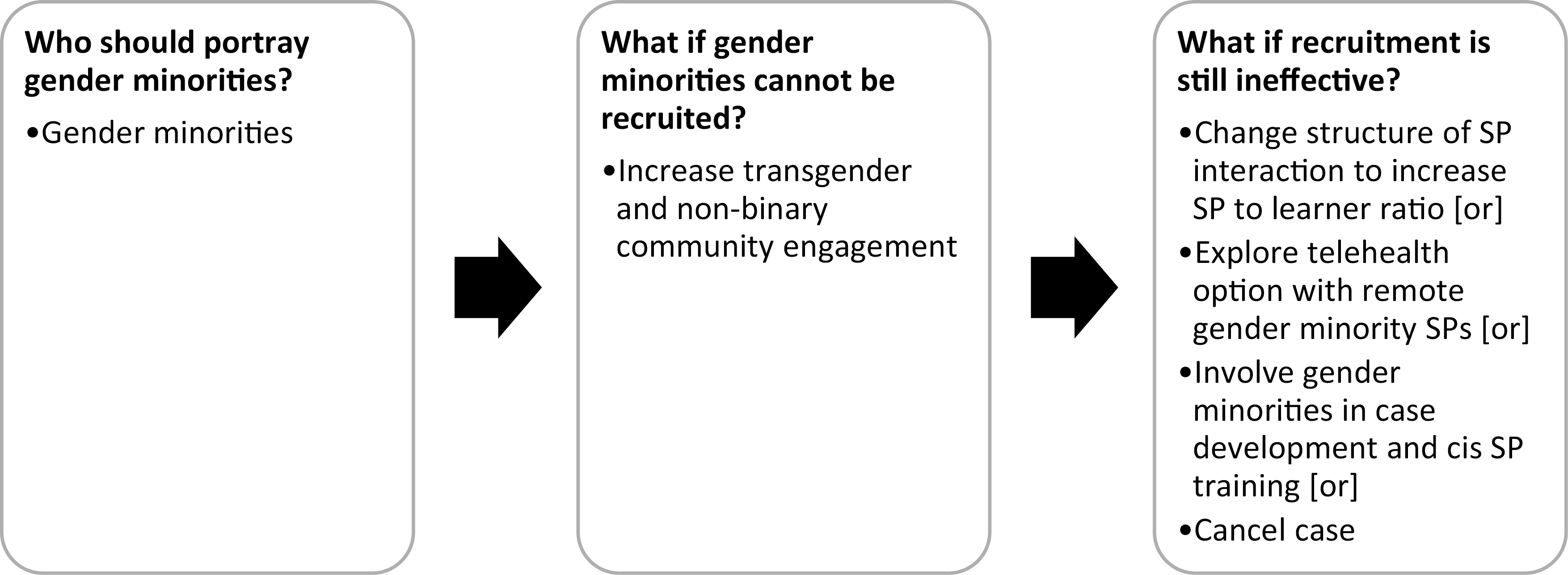
Casting gender minorities in gender minority roles is the gold standard. In situations where this is not possible, participant opinion diverged on whether it is preferable to cast cisgender simulated patients or cancel the case. Participants described gender-affirming patient simulation as impactful. They noted the potential for harm to gender minority simulated patients due to repeated learner errors.
The study provides a point of reference for educators designing simulation activities. Developing gender minority case content is important and should be undertaken with care. If recruiting gender minority simulated patients proves difficult, programs should engage their local transgender and non-binary community for input on recruitment and next steps. Increasing the simulated patient-to-learner ratio, engaging gender minority simulated patients remotely and/or involving gender minorities in case development and training may be viable alternatives.
Health disparities experienced by gender minorities (i.e. transgender and non-binary people) are an important focus in medical education. The health inequities that gender minorities experience are exacerbated by discrimination and bias in the healthcare setting [1–3]. In recent years, medical education scholars have explored ways to improve the instruction of gender minority healthcare [4–13], including through patient simulation [14–20]. A recent scoping review suggests increasing interest among medical educators in using simulation to teach gender-affirming healthcare clinical skills [21], including clinically relevant history taking, sensitive performance of physical exam and affirming communication strategies.
While literature on patient simulation and gender minorities is increasing [21], no guidelines for practice to portray diverse gender identities have been established. The literature demonstrates a range of practices are used in case authoring, simulated patient casting and simulated patient training [14,21]. While many studies do not describe the identity of their simulated patients [21], several reference assigning cisgender simulated patients in gender minority roles [22–25]. Of the articles that note cisgender simulated patients portraying gender minority patients, one article shared anecdotes ‘to highlight the stigmatization that occurs and how it can negatively impact the overall well-being of transgender individuals’, but did not report any interaction between the simulated patients and transgender people [23]. Others make no mention of specific simulated patient training on gender minority healthcare [22,24,25].
Institutions have developed approaches to gender minority simulation that are siloed from one another, leading to wide variation in practices. Current institutional differences on casting and content likely reflect leadership preferences, curricular learning objectives, resource constraints, levels of community input and stances on ethics. For example, our prior research indicates that barriers to a program’s ability to recruit gender minority simulated patients, real or perceived, and the ability to devote staff time to recruitment efforts can influence whether programs assign simulated patients to portray cases within or across gender identity [14]. Casting decisions are made almost exclusively by cisgender educators. Given their lack of lived experience, the question of ethics may have even more salience. More research is needed for simulation scholars to arrive at a set of guidelines for gender minority simulation practice [15,26].
A primary argument for using simulation methodology in healthcare education is its potential to reduce medical harm to patients [27]. Engaging in simulation sessions in which skills are actively rehearsed is found to reduce error in the field [28]. The practice of simulation itself, however, is not without the potential for harm. Instead, simulation shifts the potential for harm from actual patients to simulated patients [29]. Simulationists, therefore, must consider the ethics of these potential harms, including psychological discomfort due to tokenization and or microaggressions. Noonan et al. found that although some gender minority simulated patients experienced psychological discomfort, they perceived that the benefits of participating in simulation, such as gaining insight into medical education and increasing positive feelings of ‘hope, empowerment, and engagement’, outweighed any negative experiences [15].
Professional simulation associations, including the Association of SP Educators (ASPE), the Society for Simulation in Healthcare (SSH) and the International Nursing Association for Clinical Simulation in Learning (INACSL), provide ethical guidance through published standards and codes. In its standards of best practice, ASPE names safety and accountability as two of its core values and outlines 19 practices under the domain ‘Safe Work Practices’ [30]. These practices include several provisions for ensuring the psychological safety of participants (ASPE SOBP). SSH’s Healthcare Simulationist Code of Ethics emphasizes reducing harm, transparency, mutual respect and accountability. Each of these principles may be incorporated into the process of case design to improve protections for learners and simulated patients alike [31]. INACSL’s Code of Ethics states that the professional environment should be free from bias or discrimination [32]. Picketts et al. argue for the application of medical ethics considerations to simulation, especially when working with patients of minoritized identities [29]. These considerations include the risks and benefits of including simulation in the curriculum, the degree of curricular exposure of students prior to simulation, and mitigating the emotional impact on simulated patients.
The simulation environment, which affords learning in a time and place in which actual patients cannot be harmed, lends itself to the practice of navigating complex medical scenarios. As a result, health professions educators report utilizing simulation-based education as a tool for the exploration of medical ethics concepts. Several articles in the healthcare education literature demonstrate this application. This literature generally falls into two themes: the application of medical ethics reasoning to clinical communication, and ethical decision-making in simulation [33,34–46]. These articles, however, do not address the ethical considerations made by the authors as they established the simulated environment or tasks. This concept, the deliberate process of faculty and administrators grappling with ethical principles in the construction of simulation activities, is a newer concept in the healthcare simulation literature.
While a Healthcare Simulationist Code of Ethics and standards of best practice from simulation societies exist, they do not provide explicit guidance on ethical gender minority simulation case design. Ethical considerations are particularly important because of the widespread bias towards, and stereotyping of, gender minorities, which may influence the case content and patient portrayal. In the absence of practice guidelines to address gender minority health-centred cases in simulation, there can be no guarantee that these cases, or the simulated patients involved in them, are held to a robust ethical standard.
Our research team has completed qualitative and mixed-methods studies on gender minorities in simulation and considered the value of embodied knowledge in simulation [14,15,21,26]. We believe that additional stakeholders must be engaged to establish guidelines for practice. Gender minority individuals who are healthcare providers comprise a population of individuals with unique insight as they have experienced medical education as a student/trainee and navigated healthcare settings as a gender minority. In this paper, we describe the findings of a qualitative study of US-based gender minority providers’ perspectives on simulation for gender minority healthcare. These experiences provide a unique vantage point from which to consider ethical issues in gender minority simulation.
The aim of this study was to understand how study participants view gender minority portrayal in simulation from an ethical and pragmatic standpoint. The goal is to provide a point of reference for educators and administrators as they design their own simulation activities. Our central research questions were:
Participants were recruited through opt-in contact links at healthcare conferences and social media posts shared primarily via Facebook and Twitter from November 2020 through June 2021. Eligible subjects included US healthcare providers and trainees who (1) identify as gender minority (i.e. transgender, non-binary or any identity in which the subject’s gender identity does not match their sex assigned at birth) and (2) have previous experience with patient simulation either as a current/former health professions student who completed simulated patient encounters or a current health professions educator who is familiar with clinical skills training. Interviews were conducted in English. Gender minority healthcare providers without patient simulation experience were excluded from this study. Our study was reviewed and approved by the University of Louisville Institutional Review Board, IRB # 20.0770.
Our research team conducted 22 semi-structured interviews with eligible individuals (Table 1). Interviews focused on interviewee experience with, and perception of, simulation and gender-affirming care. Since we were most interested in stakeholder opinion of how gender minority simulation could best be practiced, we asked participants a series of questions based on different conditions for simulation (Table 2).

| Variable | Count (n = 22) |
|---|---|
| Gender identity* | |
| Trans man (incl. transmasculine, male, man of trans experience) | 12 |
| Non-binary (incl. genderqueer, agender) | 11 |
| Trans woman (incl. demi-girl, demi-woman) | 3 |
| Profession* | |
| Physician (incl. current medical students) | 9 |
| Nurse (incl. current nursing students) | 7 |
| Emergency Medical Technician | 2 |
| Physical Therapist | 2 |
| Chiropractor | 1 |
| Physician Assistant | 1 |
| Dentist | 1 |
| Simulation experience* | |
| Learner | 21 |
| Educator | 3 |
| Simulated patient | 3 |
*Respondents could choose more than one option in each category. The three participants who had experience as simulated patients were also working as, or studying to be, health professionals.

| Scenario: Case with no complicating factors | |
| Should a simulated patient’s real-life identity match the patient in the case? For example: Should trans men be portrayed by trans men? Can they be portrayed by cis men, cis women or non-binary simulated patients? etc. Please describe yes or no and why or why not |
|
| Scenario: Difficulty recruiting gender minorities and no apparent transgender and non-binary community engagement or support | |
| Some simulation programs we talked to described being unable to recruit enough gender minority simulated patients to run a case. Unless they trained cis people to portray gender minority patients, they would need to cancel the simulation. What would you do in this situation? | |
| Scenario: Difficulty recruiting gender minorities, but gender minorities engaged in case development and training | |
| One simulation professional reported that cis-simulated patients in their program effectively portray gender minority patients because their program engages gender minorities directly in the development of the patient case content and in the training of the cis-simulated patients. How would you respond this? | |
We utilized inductive thematic discourse analysis to understand and interpret these data [47]. Rather than applying predetermined codes or themes, the research team identified themes through thorough data analysis and interpretation [48–50]. The team (all authors) engaged in thematic analysis as described by Braun and Clarke [48], jointly revising codes and themes over multiple cycles.
Following a thematic analysis of our entire data set, the team used discourse analysis to closely examine interview exchanges. The practice of discourse analysis is broad, but we use the term to mean the study of talk as social action [51,52]. Language does not exist in a vacuum and observing what happens in a speech act can be a productive analysis. In other words, we wanted to know what was accomplished as part of interview talk and how interviewee perception and stance changed as the interview progressed and different scenarios were described. As Roberts and Sarangi note in their discussion of discourse analysis of medical encounters, this approach can aid in understanding ‘the unfolding argument of the whole encounter’ (p. 635) [47].
To analyse discursive exchanges, members of the research team (HD and LW) examined all the transcripts, mapping if and how each interviewee’s opinion or perception shifted when presented with new information and varying scenarios. All authors reviewed and confirmed their analysis. This analysis uncovered the tensions, emotions and problem-solving gender minority healthcare providers brought to questions about gender minority portrayal in simulation. Like Roberts and Sarangi, discourse analysis allowed us to analyse the interview ‘to show the interpretive processes and overall patterns of an activity’ (p. 632) [47].
As a research team, we believe that our respective standpoints matter in the development of our research questions and in our analysis. As such, we prioritized reflexivity and attention to our positionality in relation to the research [53,54]. Our team includes both transgender and cisgender individuals, allowing both insider and outsider knowledge about affirming or inclusive gender minority healthcare practices to be shared amongst the group. All research team members have expertise in medical education, simulation and/or gender minority health disparities.
First, we will review the core themes that we identified from our interview data: the impact of gender minority portrayal in simulation and the potential for harm to gender minorities working as simulated patients. Next, we discuss how interviewees’ stances changed as they were presented with new information about possible casting scenarios (Figure 1). Our analysis revealed that while nearly all participants agreed that cisgender people should not portray gender minority patients, this agreement diverged when varying scenarios, potential compromises and trade-offs were discussed.

Participant responses to casting scenarios
Participants considered simulation involving gender minority simulated patients and/or gender-affirming case content to be important and impactful. They described the positive impact on learners, healthcare systems, transgender and non-binary communities, and gender minority simulated patients themselves. For example, when discussing the value of gender-affirming case content on healthcare systems, one participant stated: ‘Primary care doctors… need to be able to treat patients of all gender identities and sexualities in their primary care offices, and I think having simulations that allow for gender diversity is a really big part of that’. Gender minority cases were also perceived to potentially improve relations between healthcare institutions and gender minority communities. One interviewee observed that when educational institutions hire gender minority as simulated patients, they are ‘reaffirming the fact that, like, yes, we are training our healthcare providers to be better and to do better… you’re helping them do this, but we’re also kind of rebuilding our trust and faith in you [the healthcare system]’.
Participants believed that working with gender minority simulated patients could address students’ lack of knowledge and experience, which too often sets the stage for prejudice and bias in real-world patient encounters. Many felt that learners would benefit greatly from working with gender minority simulated patients, as mistakes made in the simulated environment would help curtail them with real-life patients. For example, feedback from gender minority simulated patients could help students understand how factors such as provider verbal and body language can negatively affect a gender minority patient’s experience of a health visit. As one participant commented, ‘[gender minority simulation] would just make the cisgender students more comfortable with gender minorities and be able to talk to them without hiccups once they get into practice. It would be reducing trauma to the community at large’.
Some interviewees recognized the potential for harm to gender minority simulated patients in terms of stress and emotional burden in a formative environment. A participant said, ‘you have to find enough [gender minorities] who can either physically or virtually be present to participate and have the emotional resources to stick their necks out’. Some providers worried that programs that rely too heavily on the work of gender minority simulated patients would be perceived as a burden to the trans community: ‘I feel like minorities in any field, or any area get asked to do a lot of this work and also kind of are always being asked to step up... so there can be a burnout there as well’. In other words, participants expressed concerns about gender minority simulated patients bearing the brunt of repeated learner errors, which are commonplace and inevitable in simulation. As one participant stated, ‘we absolutely need somebody to be willing to sit through that… I don’t think that I really want to, you know, be misgendered seventeen times today. No thank you…. While I’m saying yes, I think it would be great if we had trans people playing trans roles in the training scenario… but that’s a pretty vulnerable place to put yourself’.
Participants felt strongly that simulation could have a negative impact on transgender and non-binary communities if it was not implemented with caution. Some participants described personally navigating systems of oppression, encountering stigma and discrimination, and experiencing marginalization. Simulated patients often provide one-on-one feedback to learners about the experience of being in the learner’s care. Some participants feared that cisgender simulated patients would not be trained or inherently able to identify the nuances of provider/patient interaction (e.g. such as subtle acts of discrimination). By utilizing simulated patients without lived experience, programs risk perpetuating harmful behaviours by failing to interrupt them. This question elicited emotional responses from participants, suggesting that it is necessary to implement these simulation interventions with intention and care.
Three scenarios based on our prior research [15] were presented during the interviews. The scenarios covered the appropriateness, institutional feasibility and socio-political implications of cisgender portrayal of gender minority patients (see Table 2).
Participants developed an ideological consensus regarding who should portray gender minority patients in simulated patient encounters. In response to the scenarios, most participants preferred that only individuals with a gender minority identity be offered this employment regardless of the constraints, mainly so that transgender and non-binary patients are portrayed accurately. Participants discussed the importance of authenticity in gender minority simulation education which, they argue, cisgender actors cannot deliver:
I think that there is an invaluable quality that I don’t feel a cisgender and heterosexual person can capture when portraying a sexual and gender minority. That’s my personal belief, and I’m probably biased because I’ve had these experiences and I know how significantly they have changed how I behave, how I interact, how I speak, and how I speak about myself. That, I think, is impossible to have someone who is cisgender or heterosexual portray that same experience.
Participants also suggested that assigning gender minority roles to cisgender simulated patients may be unethical. Referring to global historical and recent political debates surrounding transgender identities in schools, athletics and in healthcare, one participant stated: ‘You know in reality [cisgender people] can, but should they? No, I don’t think that they can accurately and effectively portray what it’s like to be a trans person. Especially in this world and the socio-political climate and in our country’.
The topic of assigning gender minority roles in simulation often immediately elicited strong emotional responses from interviewees. Participants typically had an immediate negative reaction to the prospect of cisgender people portraying gender minority patients in simulated patient cases. For example, one participant said, ‘it’s like my gut tells me that no, that a cis person who identifies as a cis person is not the right person to play that role’. The question of whether it is effective or appropriate for a cisgender actor to portray a gender minority patient evoked shock, anger, sarcasm, irritation and offense. As one interviewee reflected:
I think that there is obviously a lot of stigma with our identity... and so the idea of having a cisgender person who’s never experienced that trying to convey that to another cisgender person just seems utterly ridiculous to me. And how we experience our bodies. How we experience day-to-day discrimination and aggressions. How we experience perpetually having to come out and up against systems of oppression that deny us of our inherent value. How? How can a cisgender person even begin to convey all that or understand all that?
Participants referred to an institutional inability to recruit input and support from local transgender and non-binary communities as ‘a cop-out’ and ‘cis[gender] nonsense’, suggesting that an absence of gender minority engagement in simulation programs is due to an institution’s lack of effort or genuine care for the community. For example, one participant said, ‘Colleges are not hurting for money… they might think they are. I guarantee you there’s money to be found, and if [they’re] not prioritizing it, it’s because you’re not prioritizing trans lives, and that’s a… problem… I’m not sugar-coating it’.
Though all participants agreed that gender minority individuals should be given the opportunity to portray gender minority patients in simulation, a consensus was not reached about how to best realize this goal. Some participants felt that gender minority individuals should be prioritized but that cisgender simulated patients would suffice, if necessary, while others felt that there was no excuse to assign these roles to cisgender simulated patients under any circumstance. For many, this decision was complex. One participant describes that though it may be possible for a cisgender person to portray a transgender person effectively, there is still potential for harm:
I think that that’s something that is doable, it’s an achievable thing, and the idea that you could sensitively portray someone’s experience doesn’t mean that that’s not introducing a lot of potential for harm... for trans people in particular, so much of our own experiences have been shaped by having to grow up with really specific and gross media portrayals and understanding how that’s affecting us, and how it affects other people. You know? There is a lot that someone could take into that, even with good intentions, that it would be pretty traumatic to see. It could reinforce some pretty dangerous ideas about trans people.
When asked whether it was appropriate to hire cisgender simulated patients to portray gender minority experiences if no gender minority individuals were available or able to take the role, participants had a range of responses. Some participants felt that the educational subject material was important enough to move forward with the program even without gender minority participation: ‘...if it’s a choice between cancelling the case or not cancelling the case, I think I would hope that most cis people would be able to do an acceptable enough job that there would still be more educational benefit to having the case run with a cis person portraying the patient than cancelling the case entirely’. Others felt that alternative methods for educating students about gender minority healthcare should be employed before ever assigning a gender minority role to a cisgender simulated patient: ‘I think there’s a lot of material that people can look into without using cis people to play those roles’. Ultimately, the responses about who should portray gender minority patients in simulation were nuanced, multifactorial, and at times, contradictory.
In analysing the discursive exchanges, we found that, when interviewers introduced participants to the various challenges reported by simulation educators in recruiting gender minority simulated patients, roughly half of interviewees shifted their position on who should play gender minority roles. All participants expressed a clear preference for assigning gender minority roles to gender minority simulated patients, but their perspectives varied on how to optimize medical students’ learning and gender minority populations’ well-being when this was not possible. Interviewees were prompted with information about the constraints of specific patient simulation practices. For example, one program was unable to recruit gender minority simulated patients or engage sufficient gender minorities in training, thus faced the dilemma of needing cisgender people to play the role or the gender minority case would have to be cancelled altogether. Study participants were asked, under these circumstances, which would be better?
As considerations of institutional feasibility and community buy-in were introduced, many tempered their view. In one case, when prompted to consider whether cisgender actors could effectively portray gender minority experiences if hired and trained by gender minority leadership, the participant responded at first that ‘I don’t care what they say. It’s not right. It’s not going to be the same... We need to portray ourselves’. However, after further discussion, they indicated a hesitant change of opinion: ‘I think they can... I think it’s possible. I’ve seen it done in movies... And I think it has to be cis people, sometimes... such as when you are portraying a trans person before they even start hormones... I feel like I’m contradicting myself from the beginning... I hate to say it, but I think they possibly could, yeah’. In this response, we hear how the interviewee is uncertain and trying to articulate their changing position. For this subset of participants, casting cisgender people in gender minority roles was preferred to cancelling the case.
After considering the proposed scenarios and the trade-offs we introduced, some respondents said that cisgender simulated patients could portray gender minority patients under specific conditions. As such, these interviewees described extensive ‘caveats’ to their position. For example, if programs were to use cisgender simulated patients, some participants felt that gender minorities must be involved in case training: ‘What I am thinking is …. You should at the very least, if you are training cis actors, they should be trained by trans people’. Still others believed that only cisgender people with connections to transgender and non-binary communities—such as cisgender people with gender minority children or partners, or lesbian, gay or bisexual people—should portray these cases: ‘queer and trans adjacent people like my spouse… having had a front row seat to [healthcare experiences] for several years… he has that context’. When faced with a scenario such as difficulty recruiting enough gender minority simulated patients to implement a patient simulation case, most participants accepted that compromise would necessary.
A minority of interviewees organically reflected on the balance between their instinctive casting preference and the likely reality. For example, one participant concluded: ‘obviously, I think that if you can get someone who is a gender minority representing a gender minority, that’s probably ideal, but I don’t think that’s always going to be an option’.
About one-third of interviewees firmly concluded that only gender minority simulated patients should portray gender minority cases, regardless of the logistical constraints. Half of these participants were secure in this belief from the start of the interview. One interviewee described their thought process thus:
I feel like if that question were turned to something else like race or ethnicity, we would say that’s a no brainer of course. I think it’s exceedingly hard to understand the life experience, the trauma, and the discrimination that we face as trans people without being part of the community. And it would be extremely difficult or impossible for someone who really is not a trained actor to really portray that and convey that in a way that would be understood and recognized.
Ultimately, for this subset of participants, casting cisgender simulated patients for these roles was unacceptable under any circumstances.
The perspectives of gender minority healthcare providers are crucial as medical educators develop gender minority simulation cases. This cohort has both lived experience as a gender minority and familiarity with simulation in professional training; therefore, they are uniquely positioned to provide guidance on gender minority simulation practices. Participants consistently drew upon their personal experiences in both realms to explain their positions on this subject. The prevailing opinion of study participants was that casting gender minorities in scenarios featuring gender minority should be the gold standard. While several of our participants modified their position on casting when presented with real-world constraints, it is notable that some (4 of 22) remained steadfast in their view that cisgender people should never portray gender minorities in simulation. It is strongly advised that medical educators accept this position as representative of the deeply held conviction by a large sector of gender minority individuals, most of whom would not have the context of patient simulation constraints. Thus, medical educators developing gender minority simulation content must be scrupulous in their planning. It is not appropriate to cast cisgender people in gender minority roles without extensive thought, gender minority involvement in case development and training, and community buy-in.
Nonetheless, normalizing affirming, inclusive healthcare is critical for gender minority patients, so this training should not be postponed indefinitely if programs are initially challenged by imperfect circumstances. Casting challenges should not be used as an excuse to abandon medical education and assessment on these topics. Our most critical lesson for medical educators and simulationists is the vital nature of community engagement in case development and training. Our interviewees stressed that educational institutions have a duty to work collaboratively with the local transgender and non-binary community in developing curriculum. As with many diversity, equity and inclusion initiatives, diversifying the simulated patient pool and hiring community consultants to engage and inform curriculum development should be framed as continual processes [55]. Taking steps towards building relationships and diversifying the general simulated patient pool will inherently strengthen the quality of medical education in the long term by increasing student engagement with diverse individuals. Situationists should also bear in mind the unique emotional strain this work can put on gender minority SPs and take action to mitigate this harm [15].
Medical educators who lack access to enough gender minority simulated patients may wish to consider alternative approaches to achieving their aims. These include options such as changing the structure to increase the simulated patient to learner ratio [21] or exploring telehealth options with remote gender minority simulated patients from other locations. Furthermore, gender-inclusive communication should be integrated as standard practice across all healthcare topics rather than limiting it to gender minority-specific simulations. If partnership with gender minority simulated patients or community consultants is not achievable, medical educators are advised to explore training modalities other than simulation.
Gender minority simulation in medical education was widely considered by this study’s participants to be an impactful and valuable method for improving learner competence, which could ultimately contribute to better experiences for gender minority populations in healthcare broadly. The strong opinions and emotions present in participants’ responses serve as further evidence that community members’ perceived simulation as an effective intervention to address gender minority health disparities only if approached with intention, care and thoughtful community partnership.
This study had a small sample of participants based in the USA. The perspectives of gender minority healthcare providers may differ in other geographic contexts. This area of medical education has evolved rapidly over the past decade, creating a generation gap between providers who were trained before and after gender-affirming content was added to the curriculum. Indeed, most interviewees had not experienced gender minority patient simulation in their own healthcare training. Thus, the focus on practicing providers may not reflect the perspectives of current trainees or the broader medical education community. Most participants in this sample did not have simulation experience as educators, which may have hindered their ability to conceptualize the nuances of simulation design and delivery. Finally, participants were diverse in healthcare field and gender identity, which may limit its generalizability for specific disciplines. Future research should seek to understand the differences, if any, between these constituencies.
Engaging healthcare providers who are members of historically marginalized groups is an effective way to shed light on the ethical nuances of medical education decision-making. Their specialized combination of embodied, educational and professional knowledge positioned study participants as uniquely qualified to provide feedback regarding gender minority simulation in healthcare education, and especially to suggest guidelines for professional practice that honour ethics and patient experience. Overall, study participants were enthusiastic about the opportunity to draw on their lived experiences to advance our knowledge on this topic. Simulationists and medical educators should interpret this enthusiasm as a desire for accurate and affirming gender minority simulation to address health and healthcare disparities.
An analysis of our data suggests that there are both best practices and acceptable practices for engaging in gender minority patient simulation. The emerging best practice is for programs to prioritize casting gender minority simulated patients in gender minority roles due to the relevance of their lived experience to the educational environment. Our participants implored programs to exhaust all possibilities before considering cisgender casting. It is recommended that programs engage directly with local transgender and non-binary communities to recruit gender minority simulated patients. If recruitment remains ineffective, programs may need to consider cancelling the simulation, involving gender minority in case development and training, increasing gender minority simulated patient to learner ratios, pursuing telehealth options with gender minority simulated patients in other areas or employing non-simulation educational strategies. Because transgender and non-binary communities are situated in widely varying local contexts, medical educators are advised to consult with local communities to determine what trade-offs are acceptable in their context. In all cases, programs should prioritize strategies that will deliver authentic and genuinely respectful gender minority patient portrayal.
The authors wish to thank Caison Black and Luca Petrey for their contributions to this study.
None declared
None declared
None declared.
None declared.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
52.
53.
54.
55.